Dieulafoy’s lesion in the caecum as a cause of severe gastrointestinal bleeding during ulcerative colitis flare: a case report
Highlight box
Key findings
• In certain patients with ulcerative colitis and massive colonic haemorrhage emergent endoscopic therapy during colonoscopy after bowel cleansing, can be considered.
What is known and what is new?
• Emergent surgery has been the treatment of first choice for massive haemorrhage in course of ulcerative colitis flare-ups. We present an unique case in which during the flare of ulcerative colitis, the main cause of bleeding was Dieulafoy’s lesion.
What is the implication, and what should change now?
• During the diagnosis, we should not overlook rare potential causes of gastrointestinal bleeding. Colonoscopy with high quality bowel preparation can reveal more obscure causes of gastrointestinal bleeding, however, further studies are needed to validate the safety of colonoscopy performed in severe exacerbations of ulcerative colitis.
Introduction
Background
Dieulafoy’s lesion (DL) is a relatively rare but potentially life-threatening condition, as it causes 1–2% of acute gastrointestinal (GI) bleeding. The most common presenting symptom is recurrent, often massive, haematemesis associated with melaena (51%), haematemesis alone (28%), or melena alone (18%) (1). Symptom manifestation depends on location of the DL and can range from iron deficiency anaemia to life-threatening haemorrhagic shock, which has been reported to occur in up to 87% of patients with DL (2). Approximately 75–95% of DL are found within 6 cm of the gastro-oesophageal junction, predominantly on the lesser curvature of the stomach (3), but they can also be found in the duodenum (15%), oesophagus (8%), colon (2%), rectum (2%), jejunum-ileum (1%), and gastric anastomosis (1%) (4,5) The pathogenesis of DL is not clear; however, it is known that the normal gastroenteric vascular network narrows progressively as it reaches the mucosa and forms a capillary network, mostly in the submucosa, while in DL, arteriole diameter remains unchanged (1–3mm) (6). A DL is described as a protruding vessel surrounded by normal mucosa. Endoscopy plays the main role in the management of DL, including methods such as endoscopic injection sclerotherapy, thermocoagulation, and mechanical therapy (7,8). Surgical management is needed in approximately 3–16% of cases, mostly in patients with re-bleeding after undergoing endoscopic therapies (9). In ulcerative colitis (UC), massive haemorrhage is a rare manifestation. For such bleeding, emergent surgery has been the treatment of first choice (10-12).
Objective
We present a unique case in which during the flare of UC DL led to life-threatening anaemia and was successfully treated endoscopically. We present this case in accordance with the CARE reporting checklist (available at https://amj.amegroups.com/article/view/10.21037/amj-23-49/rc).
Case presentation
A 37-year-old male with UC diagnosed 10 years prior, with a history of severe flare-ups of UC requiring numerous transfusions due to life-threatening anaemia, experienced sudden onset, large volume haematochezia and melaena with haemodynamic instability.
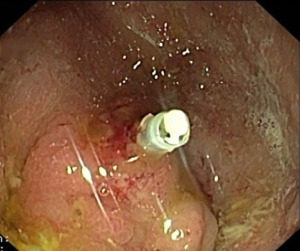
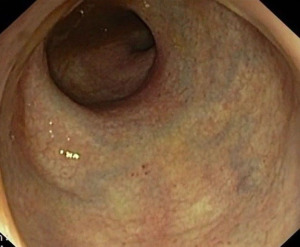
In July 2020, the patient was admitted to the hospital and his symptoms started the day prior to admission, which included melaena with bright red blood diarrhoea, vomiting, and abdominal pain. On admission, the patient presented with signs of haemorrhagic shock: systolic blood pressure was 80–100 mmHg, heart rate 130/min, hemoglobin (Hgb) level 7.8 g/dL, platelets 275×103/µL. Based on Truelove and Witts criteria (13), the exacerbation was classified as severe (>6 bloody stools per day with Hgb <10.5 g/dL and pulse >90 bpm). Intravenous fluids, along with 7 units of packed red blood cells (PRBCs) and 4 units of fresh frozen plasma (FFP) were administered in the curse of first 2 days (Table 1). The patient did not require pressor support and intensive care unit admission. Gastroscopy revealed no signs of bleeding. Abdominal radiography showed a number of fluid levels, while diagnostic abdominal ultrasound revealed right-sided bowel with enlarged walls, surrounded by swollen adipose tissue. Additionally, sigmoidoscopy was performed, revealing a mucosal appearance suggestive of mild disease activity (Mayo endoscopic score 1). Endoscopic examination did not reveal cause of extensive bleeding. After receiving intensive fluid therapy, intravenous corticosteroid (400 mg of hydrocortisone daily) and 5-aminosalicylates (4 g mesalazine daily) for the next 3 days, our patient was hemodynamically stable, afebrile, and had no signs of severe inflammation. Moreover, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and white blood cell (WBC) were within reference range. However, rectal bleeding was still present, requiring further PRBC transfusions. Because of this, and the fact that there were no radiological signs of toxic megacolon, the patient underwent full colonoscopy after bowel preparation using macrogol which confirmed left-sided colitis with mild to moderate disease activity (Mayo endoscopic score 1–2) (Figure 1). Furthermore, in the caecum, a DL was discovered—a protruding vessel with visible clot surrounded by normal mucosa—hemoclip was applied (Figures 2-4). After the procedure, the patient experienced no further haematochezia and was discharged from the hospital. In total, the patient received 19 units of PRBCs, 6 units of FFP, and 20 units of cryoprecipitate in the course of 6 days. Neither adverse nor unanticipated events happened after the procedure.
Table 1
| Day of care | Diagnostic procedure | Therapy |
|---|---|---|
| Admission—Day 1 | Abdominal radiography, abdominal diagnostic ultrasound | Intravenous fluids: 4 units of PRBCs; 2 units of FFP. 400 mg of hydrocortisone intravenously; 4 g mesalazine orally |
| Day 2 | Sigmoidoscopy | Intravenous fluids: 3 units of PRBCs; 2 units of FFP; 10 units of cryoprecipitate. 400 mg of hydrocortisone intravenously; 4 g mesalazine orally |
| Day 3 | Gastroscopy, abdominal diagnostic ultrasound | Intravenous fluids: 4 units of PRBCs; 2 units of FFP; 5 units of cryoprecipitate. 300 mg of hydrocortisone intravenously; 4 g mesalazine orally |
| Day 4 | – | Intravenous fluids: 4 units of PRBCs; 5 units of cryoprecipitate. 300 mg of hydrocortisone intravenously; 4 g mesalazine orally |
| Day 5 | Abdominal radiography | Intravenous fluids: 2 units of PRBCs. 300 mg of hydrocortisone intravenously; 4 g mesalazine orally |
| Day 6 | Colonoscopy | Intravenous fluids: 2 units of PRBCs. 40 mg prednizone oraly; 4 g mesalazine orally |
| Day 9 | Discharge from the hospital | – |
PRBCs, packed red blood cells; FFP, fresh frozen plasma.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
DL bleeding is often massive and leads to hypovolemic shock. In presented case, the patient was diagnosed with UC, in which haematochezia often occurs as one of the manifestations which can be caused by extensive disease activity. Nevertheless, severe lower GI bleeding leading to hypovolemic shock is a rare manifestation of UC and is limited mostly to exacerbated disease or fulminant colitis (10). Emergency proctocolectomy is the only reliable treatment in this group of patients (11). In our patient, sigmoidoscopy was performed, revealing only mild disease activity in mucosal appearance (Mayo endoscopic score 1), which did not correspond with the massive bleeding. Colonoscopy showed DL in the caecum. After the application of one hemoclip, no further episodes of bleeding were observed and the patient was discharged from the hospital.
Strengths and limitations
Presented study shares limitations with other representatives of case report genre: it applies to a small number of patients, has low generalizability. However, because clinical medical learning is to a large degree case-based, we believe that our study will help in day-to-day clinical practice, as an educational tool. It emphasizes the importance of thorough diagnostic evaluation, to not overlook the rarest possible causes of patient symptoms.
Comparison with similar researches
In the literature, there are only a few other case reports of patients with inflammatory bowel disease (IBD) and extensive bleeding caused by DL, but they pertain to patients with both clinical and endoscopical remission of UC (14,15). Therefore, we describe a unique case in which DL led to life-threatening anaemia during the flare of UC and was successfully treated endoscopically.
Implications and actions needed
There is currently a lack of prospective studies which would validate the safety of performing colonoscopy in severe flare-ups of UC. While sigmoidoscopy is commonly performed during severe exacerbations of UC and is considered to be sufficient for assessing disease severity, it is avoided until the disease activity has decreased, mainly due to the fear of complications such as perforation during severe flare-ups. To validate this practice, Carbonnel et al. demonstrated that colonoscopic examination is safe in acute flare-ups of UC; however, it is important to note that endoscopic procedures in this study group were performed by an experienced colonoscopists (16).
Endoscopic procedures are the treatment of choice in patients with DL, with success rates exceeding 90% (17). Endoscopic haemostasis is achieved with thermal or argon plasma coagulation, local injection of epinephrine and mechanical therapy such as banding and hemoclipping. The risk of re-bleeding from DL has been reported to vary anywhere between 9–40% and this risk has been found to be higher in endoscopic monotherapy when compared with combined endoscopic therapies (4,18). Despite the lack of studies, endoscopical haemostatic procedures seem to be less safe when performed in severe exacerbations of IBD, because of the high risk of perforation. Nevertheless, in certain group of patients, it could be considered as an alternative for surgery.
Conclusions
In summary, although haematochezia is a well-known manifestation of UC, we should not overlook other potential causes of GI bleeding. Colonoscopy with high quality bowel preparation can reveal more obscure causes of GI bleeding when compared to sigmoidoscopy performed without bowel cleansing. However, further studies are needed to validate the safety of colonoscopy performed in severe exacerbations of UC.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://amj.amegroups.com/article/view/10.21037/amj-23-49/rc
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-23-49/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-23-49/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Reilly HF 3rd, al-Kawas FH. Dieulafoy’s lesion. Diagnosis and management. Dig Dis Sci 1991;36:1702-7. [Crossref] [PubMed]
- Nguyen DC, Jackson CS. The Dieulafoy’s Lesion: An Update on Evaluation, Diagnosis, and Management. J Clin Gastroenterol 2015;49:541-9. [Crossref] [PubMed]
- Katz PO, Salas L. Less frequent causes of upper gastrointestinal bleeding. Gastroenterol Clin North Am 1993;22:875-89. [Crossref] [PubMed]
- Baxter M, Aly EH. Dieulafoy’s lesion: current trends in diagnosis and management. Ann R Coll Surg Engl 2010;92:548-54. [Crossref] [PubMed]
- Dogan U, Gomceli I, Koc U, et al. Rectal dieulafoy lesions: a rare etiology of chronic lower gastrointestinal bleeding. Case Rep Med 2014;2014:180230. [Crossref] [PubMed]
- Shin HJ, Ju JS, Kim KD, et al. Risk Factors for Dieulafoy Lesions in the Upper Gastrointestinal Tract. Clin Endosc 2015;48:228-33. [Crossref] [PubMed]
- Khan R, Mahmad A, Gobrial M, et al. The Diagnostic Dilemma of Dieulafoy’s Lesion. Gastroenterology Res 2015;8:201-6. [Crossref] [PubMed]
- Wang Y, Bansal P, Li S, et al. Dieulafoy’s lesion of the upper GI tract: a comprehensive nationwide database analysis. Gastrointest Endosc 2021;94:24-34.e5. [Crossref] [PubMed]
- Inayat F, Ullah W, Hussain Q, et al. Dieulafoy’s lesion of the oesophagus: a case series and literature review. BMJ Case Rep 2017;2017:bcr2016218100. [Crossref] [PubMed]
- Pardi DS, Loftus EV Jr, Tremaine WJ, et al. Acute major gastrointestinal hemorrhage in inflammatory bowel disease. Gastrointest Endosc 1999;49:153-7. [Crossref] [PubMed]
- Mallant-Hent RCh, van Bodegraven AA, Meuwissen SG, et al. Alternative approach to massive gastrointestinal bleeding in ulcerative colitis: highly selective transcatheter embolization. Eur J Gastroenterol Hepatol 2003;15:189-93. [Crossref] [PubMed]
- Edwards FC, Truelove SC. Course and prognosis of ulcerative colitis. III Complications. Gut 1964;5:1-22. [PubMed]
- Truelove SC, Witts LJ. Cortisone in ulcerative colitis; preliminary report on a therapeutic trial. Br Med J 1954;2:375-8. [Crossref] [PubMed]
- Tang D, Lin J. A Case of Ileal Dieulafoy’s Lesion in a Patient with Crohn’s Disease: 789. Am J Gastroenterol 2006;101:S318. [Crossref]
- Bielicki D, Wasilewicz MP. Acute lower gastrointestinal tract bleeding caused by Dieulafoy lesion in rectum—case report. Pol Merkur Lekarski 2006;20:708-9. [PubMed]
- Carbonnel F, Lavergne A, Lémann M, et al. Colonoscopy of acute colitis. A safe and reliable tool for assessment of severity. Dig Dis Sci 1994;39:1550-7. [Crossref] [PubMed]
- Dulic-Lakovic E, Dulic M, Hubner D, et al. Bleeding Dieulafoy lesions of the small bowel: a systematic study on the epidemiology and efficacy of enteroscopic treatment. Gastrointest Endosc 2011;74:573-80. [Crossref] [PubMed]
- Lee YT, Walmsley RS, Leong RW, et al. Dieulafoy’s lesion. Gastrointest Endosc 2003;58:236-43. [Crossref] [PubMed]
Cite this article as: Czyż P, Filip R. Dieulafoy’s lesion in the caecum as a cause of severe gastrointestinal bleeding during ulcerative colitis flare: a case report. AME Med J 2023;8:27.