Airway stent associated respiratory tract infections
Introduction
Central airway obstruction (CAO) can be from malignant and non-malignant diseases. Malignant etiology is more common of the two and is reported in the literature up to 20–30% of lung cancers (1). Airway stents are effective in the treatment of airway obstruction; although not definitive therapy, they can be used as bridge to therapy or a palliative approach. Airway stenting is effective in alleviating symptoms, but complications related to airway stenting are not uncommon. Immediate perioperative complications are rare but long-term complications are common and are more serious (2,3). Lower respiratory tract infection (LRTI), granulation tissue, mucus plugging, stent migration, and stent fracture are possible long-term complications from airway stenting. AQuiRE registry was the largest study that specifically addressed stent related complications and therapeutic bronchoscopy, and found the procedural complication rate to be only 3.9% with 0.5% resulting in death (4). There is a wide range of stent-related complication rates reported in the literature due to heterogeneous patient population and the types of airway stents used, with an overall infection rate of 19% reported in a systematic review (3). The largest studies summarizing this data can be found in Table 1.
Table 1
| Authors and year | Type of study and time frame | Patient population | LRTI rate | Other |
|---|---|---|---|---|
| Agrafiotis et al. (3), 2009 | Systemic review | 19 cohorts; 4 case reports; 501 patients | 19%; most common pathogens: Staphylococcus aureus and Pseudomonas aeruginosa; 68% mortality rate | – |
| Grosu et al. (5), 2013 | Retrospective, September 2009–August 2011 | Malignant airways disease, N=72; 24 patients received one or more stents | 32%; hazard ratio of infection (stent: no stent) 3.76; 95% CI: 1.57–8.99; P=0.003 | – |
| Ost et al. (6), 2012 | Retrospective | Malignant airway disease, N=172; 195 stents in total [Ultraflex: 118; Aero: 31; Dumon Silicone (Y/Straight): 46] | Median time to infection: 1 month; aero stent: increased risk of infection; 23%: died of respiratory infection within 14 days of infection | Time to complications: ~1–1.4 months |
| Zhang et al. (7), 2016 | Prospective nested case-control, January 2011–March 2015 | 103 patients | 27.2%; most common pathogens: Staphylococcus aureus and Pseudomonas aeruginosa | Favorable risk factor: female gender; age <50 years |
LRTI, lower respiratory tract infection; CI, confidence interval.
Epidemiology
Grosu et al. compared the incidence rates of infection in patients who underwent therapeutic bronchoscopy for malignant airway obstruction, and found stents were associated with an increased risk of infection [hazard ratio (HR), 3.76; 95% confidence interval (CI): 1.57–8.99; P=0.003] (5). The incidence rate of LRTI was 0.0057 infections per person-day in patients with stents vs. 0.0011 infections per person-day in patients without stents. The incidence rate difference, 0.0046 infections per person-day, was significant (95% CI: 0.0012–0.0081; P=0.0002), and translates into a 13% increased risk of LRTI per month, equal to one infection for every 8 stents placed. 26% of the study patients with infections died within 2 weeks of the stent placement (5).
Ost et al. conducted a retrospective comparing various airway stents in patients with malignant airway obstruction from January 2005 to August 2010. One hundred and seventy-two patients with 195 stent procedures were included. They found 106 LRTI in 73 patients, with a median time to infection being 1 month. More than half of these patients with LRTI were hospitalized, and 23% of them died within two weeks of their infection. The cause of death was not specified for these patients, however. The authors mentioned that left sided stents, stents for compression/barrier and LRTI were associated with increased mortality. With regards to stent type, the incidence rate of stent infections was double for Aero compared to other stents (HR =1.98; 95% CI: 1.03–3.81; P=0.041). Silicone stents (HR =3.32; 95% CI: 1.59–6.93; P=0.001) and LRTIs (HR =5.69; 95% CI: 2.60–12.42; P<0.001) increased the risk of granulation tissue. Respiratory infections were found to be associated with decreased survival (HR =1.57; 95% CI: 1.11–2.21; P=0.011) (6).
Agrafiotis et al. [2009] performed a systematic review to report the evidence on infections related to airway stenting. Twenty-three reports involving 501 patients with airway stents were included. They found that 19% of the stented patients experienced stent-associated respiratory tract infection (SARTI), with pneumonia being the most common infection followed by bronchial infection, cavitary pneumonia/lung abscess or intraluminal fungus ball (Figure 1). Infection was based on microbiologic confirmation. The most common pathogens were Staphylococcus aureus and Pseudomonas aeruginosa. The mortality rate of SARTI was high (68%). The authors concluded that SARTI is a common and serious complication of airway stenting and suggested the need for a consensus definition and diagnostic criteria for SARTI (3). A prospective case-control study by Zhang et al. [2016] evaluated the incidence and predictive risk factors of SARTI. They included 103 total patients and found an incidence of SARTI of 27.2% (28/103). There was no difference in the incidence of SARTI between stent types and shapes of stents. The most common pathogens were Staphylococcus aureus (50%) and Pseudomonas aeruginosa (35.7%). Time to infection for Staphylococcus aureus was 7 (range, 4–60) days, while time for infection with Pseudomonas aeruginosa was 53 (range, 15–67) days. Favorable predictive factors for SARTI included female sex and younger age below 50 years old (7).
In 2018, Huang et al. conducted a retrospective single center cohort study of lung cancer and esophageal cancer for patients who received stent placement for malignant airway lesions to assess stent related complications. Fifty-six patients underwent 66 stent procedures (29 in the lung cancer group, 27 in the esophageal cancer group). Only two patients in the lung cancer group and one in the esophageal cancer group developed stent related infection. The esophageal cancer patient with SARTI had a prolonged procedure duration (>110 minutes), but analysis is limited by small sample size (8).
The above data highlights the heterogeneity in the published literature for incidence of SARTI which might be attributable to a difference in how SARTI is defined, and symptom overlap in patient with SARTI and other pulmonary disease processes.
Pathogenesis
Bacterial colonization and biofilm formation are though to play a significant role in stent related infections. In a small 39 patient study who underwent airway stenting for benign and malignant stenosis, bacterial colonization of airway stents was found in 87.5% of patients after 12 months. The most frequent microorganisms were Staphylococcus aureus and Pseudomonas aeruginosa. These bacteria were also associated with a higher risk of developing airway granulation, which can cause further narrowing of the airway and bleeding (9). Vitsas et al. found that out of 24 airway stents placed (16 silicone, 8 metal), 14/24 (58%, 12 silicone stents, 2 metal stent) were positive for a pathogen on bronchial washing, but only three patients required antibiotics for true infection. Pseudomonas aeruginosa followed by Klebsiella pneumonia were the most commonly encountered bacteria (10). In a prospective study by Noppen et al. where they performed protected brush specimen sampling of the airway before and after stent placement, as high as 78% of stents were colonized within 3–4 weeks of implantation (11). Gottlieb and colleagues analyzed complications in lung transplant recipients who underwent self-expandable metallic stents (SEMS) [65 (9.2%) out of 706 recipients, underwent 111 (91% noncovered) bronchial SEMS]. New bacterial airway colonization occurred after SEMS insertion in 40% of the patients with 5-year survival significantly lower (60% vs. 76%; P=0.02). Re-stenosis and airway colonization were major late complications (12).
Biofilms have been recognized in other implants related infections (ureteral stents, central lines, biliary stents) and similar mechanisms are likely in the respiratory tract. A recent study of airway stents found that the stent biofilm type was significantly correlated with stent material: covered metal with the Staphylococcus-type biofilm, silicone with the Corynebacterium-dominated biofilm, and uncovered metal with the polymicrobial biofilm. Subjects with sequential stents had frequent transitions between community types. Fungal analysis found Candida was most prevalent (13).
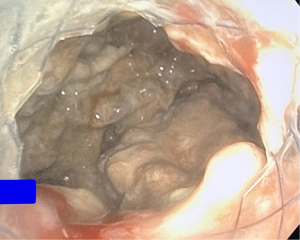
Another hypothesis suggests impaired ciliary function from the radial compression of stent on the airway leading to mucus accumulation and infection thereafter (Figures 2,3). It has been previously found that sterilization did not affect stent associated airway infection given that there was no difference in the infection rate between non sterilized ultra-flex stent and the sterilized silicone stents. Instead, they suggested that the stent design or the way the stents were manufactured made the difference in infection rate. Interestingly, Aerostents were manufactured with inner lumen hydrophilic coating to prevent mucostasis but is found to have the highest infection risk (6). It is unclear if this protective coating increases or decreases the infection risk. Multiple studies found coalition between airway granulation, polymicrobial colonization and respiratory infections. Polymicrobial colonization is associated with increased granulation tissue which can lead to infections, or obstruction from granulation tissue results in infection (14,15).
Diagnosis
Currently there is no solidarity on the diagnostic criteria for SARTI. Acceptable criteria from the multiple authors include constitutional symptoms of fever, chills, and increased sputum production and purulence, with or without evidence of pneumonia or lung abscess and microbacterial cultures (6). We believe this is a reasonable definition and would encourage treatment based on clinician discretion rather than solely on strict criteria requiring radiographic correlation. Pathogenesis includes impaired ciliary function from the radial compression of stent on the airway leading to mucus accumulation and thereafter infection (Figures 2,3).
Prevention and treatment
Airway stenting practices vary widely by region. A recent international survey within 26 European counties on airway stent practices found significant heterogeneity in regard to the type of anesthesia used, bronchoscopy type (rigid vs. flexible), type of stent used, and the personnel performing the therapeutic bronchoscopy. The authors hypothesized that the variations could be from the difference in the level of training and reimbursement pattern in different health care systems (16).
With regards to preventing or reducing airway stent infections and colonization several strategies have been proposed. These include antibiotic prophylaxis, antimicrobial coating of stents, regular bronchoscopic cleaning of stents, and removal or replacement of infected stents. Matsuo et al. did not find that routine surveillance bronchoscopy after stent insertion in asymptomatic patients resulted in early detection of stent related complications (17). Contrary to the prior study, a more recent study by Lee et al. assessed the utility of surveillance bronchoscopy. This was a retrospective cohort of 94 surveillance bronchoscopies in 134 patients, in which 147 stents were placed for benign or malignant disease. Bronchoscopy was done 4–6 weeks post stenting or earlier if symptomatic. They found that routine surveillance bronchoscopy may have utility in early detection of stent associated airway complications and help delay post-obstructive pneumonia and respiratory failure. Of the three stent materials used (metallic, silicone, hybrid), hybrid stents were more likely to migrate or obstruct secretions. Additionally, they could not determine if this practice could impact mortality, morbidity, length of hospitalization and the health care burden (18).
A French survey was sent to interventionalists regarding prophylactic antibiotics before and after airway stenting. Of thirty-six participants, 86% did not use prophylactic antibiotics before airway stenting, and 68% did not use them after airway stent; 30% however did use prophylactic antibiotics post airway stent in high-risk situations such as chronic respiratory failure, or immunosuppression such as lung transplant and active cancer treatment (19).
A recent United States survey to understand post-stent management strategies found that the practice varied markedly in the country. At least one medication was prescribed by 75% of the practitioners to prevent post-endobronchial stent infection. Routine surveillance bronchoscopy was done by 53%, mucociliary clearance regimens were prescribed by 26%, and routine imaging was done by 17%; 8.3% replaced the stents routinely (20). None of the above strategies have been fully elucidated, and practice varies among individuals.
The treatment of airway stent infections and colonization depends on the type and severity of the infection, the underlying cause of the airway obstruction, the type and material of the stent, and the patient’s condition and preferences. The main goals of treatment are to eradicate the infection, relieve symptoms, preserve the patency of the stent, and avoid complications. Treatment options include systemic or topical antibiotics, bronchoscopic debridement or lavage of the stent, removal or exchange of the stent, or additional interventions such as laser therapy, cryotherapy, or balloon dilation. The choice of treatment should be individualized and based on a multidisciplinary assessment of each case.
Overall, there is no consensus on the optimal approach, and the evidence for the efficacy and safety of these interventions is limited. Moreover, some of these strategies may have adverse effects, such as antibiotic resistance, toxicity, or damage to the stent or the airway wall. Until data is available regarding prophylactic antibiotics, differentiating colonization from true infection will remain important in post-airway stenting management. When true infection is present, timely antibiotics may limit further complications. There is definitely an urgent need for a diagnostic criteria and definition of airway stent associated respiratory infections
Future direction
3D stents: in the era of personalized medicine, patient specific individualized airway stents for airway specific conditions using 3D printing have been developed recently hoping to minimize complications and the need for repeat interventions. Since 2015 there have been multiple case reports and case series reported, most with benign lesions using silicone stents. Guibert et al. used 3D stents for patients with anatomically complex airway stenosis in 10 patients and found a 3-month complication rate of 40%. Complications included mucus plugging, migrations, and cough. No infections were reported (21). Shan et al. assessed 3D printed airway stents in malignant laryngotracheal stenosis in 10 patients. All patients had symptomatic relief, with restenosis occurring in 2 patients between 3- and 5-month post stenting, mucus retention in 3 patients, and stent migration in 1 patient. No SARTI were reported (22). Currently the complications from 3D stents seem to be acceptable with a low infection risk from available data but larger randomized studies are necessary to comment on the safety profile.
Drug eluting stents (DES): sustained drug release from these stents could inhibit granulomatous tissue formation and possibly reduce infections. A recent study by Debiane et al. randomly assigned pigs to DES and traditional silicone stents and found no difference in the amount of granulation tissue, but noticed that the DES stents demonstrated antimicrobial activity (23). Similarly, Wang et al. found reduced granulation tissue in experimental group with paclitaxel DES compared to standard stents in beagles (24). Currently there is limited data available, with the majority of them are in animal models. Mitomycin C and sirolimus administration locally post stent placement was shown to reduce granulation formation in small studies (25,26). There are multiple studies that are currently looking into DES with cytotoxic drugs including paclitaxel and cisplatin. Silicone rubber stents infused with paclitaxel reduced interleukin-8 (IL-8) levels in cancer cell lines, which may suppress growth of granulation tissue (27).
Biodegradable stents: despite data being limited to animal models and small case studies, these stents have gained interest lately because they can degrade slowly, thereby reducing stent associated complications. The largest study by Lischke et al. reported insertion of 20 biodegradable stents in post-transplant bronchial stenosis with good outcomes (28). Fuehner et al. observed satisfactory results as well in their small cohort of 11 biodegradable stents in 10 lung transplant patients with all patients free from further airway intervention for 6 months; 100% survival was seen (29). Biodegradable stents were also combined with DES in an animal study using biodegradable cisplatin eluding stents. Stent strength was comparable to self-expandable stents, and cisplatin release occurred over 5 weeks. These provided encouraging data, however clinical efficacy still needs to be determined for these agents (30). Animal model data is available on mitomycin C bioabsorbable with stents as well showing promising results (31).
Radioactive stents: a recent metanalysis by Meng et al. found that radioactive stents were associated with higher survival rates and reduced stent restenosis rate compared to normal stents in treating malignant airway stenosis (32).
There is no data regarding the utility of inhaled antibiotics to prevent or treat SARTI. Most data on inhaled antibiotics are regarding cystic fibrosis related bronchiectasis, with limited and conflicting data for non-cystic fibrosis bronchiectasis. Inhaled antibiotic use for SARTI will likely be a topic for further investigation (33). Silver has high antimicrobial activity, and its usage has been well documented in the literature. Silver coated endobronchial stents could possibly be of utility in the future as they exhibit antimicrobial activity thereby reventing biofilm formation and reducing infections (34).
Conclusions
Airway stent infections and colonization are common complications in patients treated for airway obstruction. LRTI associated with airway stents can lead to increased morbidity, mortality, and health care costs. Stent colonization with microbacterial biome is much more common than actual infections and there are no consensus criteria to delineate the transition from colonization to infection. Emerging data suggests that the stent design and type might have a role in pathogenesis. The protocols for diagnosis, prevention as well as treatment vary widely between institutions which can impede progress towards developments of standardized protocols.
Airway stent infections and colonization are challenging complications that require careful monitoring and management. More research is needed to establish the definition and best practices for preventing and treating these conditions in patients with airway stents. Further studies investigating antibiotic impregnated airway stents could reduce airway infections are warranted. DES and biodegradable stents may be helpful in reducing granulation tissue and thereby ultimately reducing the infection risk, but further data is needed.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jonathan Kurman and Bryan S. Benn) for the series “Diagnostic & Therapeutic Bronchoscopy” published in AME Medical Journal. The article has undergone external peer review.
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-23-117/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-23-117/coif). The series “Diagnostic & Therapeutic Bronchoscopy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Murgu SD, Egressy K, Laxmanan B, et al. Central Airway Obstruction: Benign Strictures, Tracheobronchomalacia, and Malignancy-related Obstruction. Chest 2016;150:426-41. [Crossref] [PubMed]
- Ernst A, Simoff M, Ost D, et al. Prospective risk-adjusted morbidity and mortality outcome analysis after therapeutic bronchoscopic procedures: results of a multi-institutional outcomes database. Chest 2008;134:514-9. [Crossref] [PubMed]
- Agrafiotis M, Siempos II, Falagas ME. Infections related to airway stenting: a systematic review. Respiration 2009;78:69-74. [Crossref] [PubMed]
- Ost DE, Ernst A, Grosu HB, et al. Complications Following Therapeutic Bronchoscopy for Malignant Central Airway Obstruction: Results of the AQuIRE Registry. Chest 2015;148:450-71. [Crossref] [PubMed]
- Grosu HB, Eapen GA, Morice RC, et al. Stents are associated with increased risk of respiratory infections in patients undergoing airway interventions for malignant airways disease. Chest 2013;144:441-9. [Crossref] [PubMed]
- Ost DE, Shah AM, Lei X, et al. Respiratory infections increase the risk of granulation tissue formation following airway stenting in patients with malignant airway obstruction. Chest 2012;141:1473-81. [Crossref] [PubMed]
- Zhang JL, Zou H, Wang HW, et al. Incidence, bacterial spectrum and predictive risk factors for stent associated respiratory tract infection. Zhonghua Jie He He Hu Xi Za Zhi 2016;39:368-71. [PubMed]
- Huang S, Xu J, An Z, et al. Clinical assessment of airway stent placement in patients with malignant airway lesions. J Thorac Dis 2018;10:3277-88. [Crossref] [PubMed]
- Cascόn RP, Lisbona RL, Cubero de Frutos N, et al. Incidence of bacterial colonization in patients with tracheobronchial stents. Eur Respir J 2011;38:616.
- Vitsas V, Touman A, Agelakis L, et al. Bacterial colonization/infection of the airway stents. Eur Respir J 2017;50:PA3792.
- Noppen M, Piérard D, Meysman M, et al. Bacterial colonization of central airways after stenting. Am J Respir Crit Care Med 1999;160:672-7. [Crossref] [PubMed]
- Gottlieb J, Fuehner T, Dierich M, et al. Are metallic stents really safe? A long-term analysis in lung transplant recipients. Eur Respir J 2009;34:1417-22. [Crossref] [PubMed]
- McGinniss JE, Imai I, Simon-Soro A, et al. Molecular analysis of the endobronchial stent microbial biofilm reveals bacterial communities that associate with stent material and frequent fungal constituents. PLoS One 2019;14:e0217306. [Crossref] [PubMed]
- Nouraei SA, Petrou MA, Randhawa PS, et al. Bacterial colonization of airway stents: a promoter of granulation tissue formation following laryngotracheal reconstruction. Arch Otolaryngol Head Neck Surg 2006;132:1086-90. [Crossref] [PubMed]
- Schmäl F, Fegeler W, Terpe HJ, et al. Bacteria and granulation tissue associated with Montgomery T-tubes. Laryngoscope 2003;113:1394-400. [Crossref] [PubMed]
- Dutau H, Breen D, Bugalho A, et al. Current Practice of Airway Stenting in the Adult Population in Europe: A Survey of the European Association of Bronchology and Interventional Pulmonology (EABIP). Respiration 2018;95:44-54. [Crossref] [PubMed]
- Matsuo T, Colt HG. Evidence against routine scheduling of surveillance bronchoscopy after stent insertion. Chest 2000;118:1455-9. [Crossref] [PubMed]
- Lee HJ, Labaki W, Yu DH, et al. Airway stent complications: the role of follow-up bronchoscopy as a surveillance method. J Thorac Dis 2017;9:4651-9. [Crossref] [PubMed]
- Virot E, Marcot C, Vergnon JM, et al. Airway stent current practices evaluation: Survey among French bronchoscopy practitioners. Respir Med Res 2020;77:89-94. [Crossref] [PubMed]
- Wayne MT, Ali MS, Wakeam E, et al. Current Practices in Airway Stent Management: A National Survey of US Practitioners. Respiration 2023;102:608-12. [Crossref] [PubMed]
- Guibert N, Didier A, Moreno B, et al. Treatment of complex airway stenoses using patient-specific 3D-engineered stents: a proof-of-concept study. Thorax 2019;74:810-3. [Crossref] [PubMed]
- Shan Q, Huang W, Wang Z, et al. Preliminary Experience With a Novel Metallic Segmented Transcordal Stent Modified With Three-Dimensional Printing for Inoperable Malignant Laryngotracheal Stenosis. Front Oncol 2021;11:619781. [Crossref] [PubMed]
- Debiane L, Reitzel R, Rosenblatt J, et al. A Design-Based Stereologic Method to Quantify the Tissue Changes Associated with a Novel Drug-Eluting Tracheobronchial Stent. Respiration 2019;98:60-9. [Crossref] [PubMed]
- Wang T, Zhang J, Wang J, et al. Paclitaxel Drug-eluting Tracheal Stent Could Reduce Granulation Tissue Formation in a Canine Model. Chin Med J (Engl) 2016;129:2708-13. [Crossref] [PubMed]
- Li F, Li P, Cai Z, et al. Establishment of two canine models of benign airway stenosis and the effect of mitomycin C on airway stenosis. Int J Pediatr Otorhinolaryngol 2022;159:111205. [Crossref] [PubMed]
- Motz KM, Lina IA, Samad I, et al. Sirolimus-eluting airway stent reduces profibrotic Th17 cells and inhibits laryngotracheal stenosis. JCI Insight 2023;8:e158456. [Crossref] [PubMed]
- Xu J, Ong HX, Traini D, et al. Paclitaxel-eluting silicone airway stent for preventing granulation tissue growth and lung cancer relapse in central airway pathologies. Expert Opin Drug Deliv 2020;17:1631-45. [Crossref] [PubMed]
- Lischke R, Pozniak J, Vondrys D, et al. Novel biodegradable stents in the treatment of bronchial stenosis after lung transplantation. Eur J Cardiothorac Surg 2011;40:619-24. [Crossref] [PubMed]
- Fuehner T, Suhling H, Greer M, et al. Biodegradable stents after lung transplantation. Transpl Int 2013;26:e58-60. [Crossref] [PubMed]
- Chao YK, Liu KS, Wang YC, et al. Biodegradable cisplatin-eluting tracheal stent for malignant airway obstruction: in vivo and in vitro studies. Chest 2013;144:193-9. [Crossref] [PubMed]
- Zhu GH, Ng AH, Venkatraman SS, et al. A novel bioabsorbable drug-eluting tracheal stent. Laryngoscope 2011;121:2234-9. [Crossref] [PubMed]
- Meng QK, Yu XY, Li W, et al. Radioactive and normal stent insertion for the treatment of malignant airway stenosis: A meta-analysis. Brachytherapy 2021;20:883-91. [Crossref] [PubMed]
- Quon BS, Goss CH, Ramsey BW. Inhaled antibiotics for lower airway infections. Ann Am Thorac Soc 2014;11:425-34. [Crossref] [PubMed]
- Diez-Ferrer M, Marti S, Calatayud L, et al. In vitro evaluation of silver-coated silicone tracheobronchial stents on growth and attachment of clinical isolates. Eur Respir J 2014;44:700.
Cite this article as: Madisi NY, Greenberg D, Balwan A. Airway stent associated respiratory tract infections. AME Med J 2024;9:3.