Robotic-assisted thoracoscopic thymectomy
Clinical data
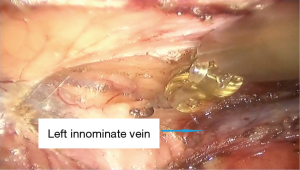
A 68-year-old woman was referred to our hospital because of a chest computed tomography (CT) scan showing an abnormal shadow in the anterior mediastinum. She had no obvious symptoms except for a slight cough on exertion for a year. She had undergone an appendectomy and a fracture of the left tibia and fibula 16 years previously. Chest CT-scan showed a well-defined mass (18 mm × 12 mm) in the anterior mediastinum, in contact with left innominate vein (Figure 1). The homogenous contrast effect of the tumor had increased compared with itself half a year ago. The pulmonary function and other laboratory tests were normal. Differential diagnosis included thymoma, thymic carcinoma, and mediastinal cyst; therefore, surgical resection was recommended. Preoperative needle biopsy was not performed because of the deep location of the tumor. Informed consent for robotic-assisted thoracic lobectomy was obtained from patient before operation.
Procedure
We used two arms of the Da Vinci Robotic System and a 30° camera for thymectomies. The patient was anesthetized and intubated with a double-lumen endotracheal tube.
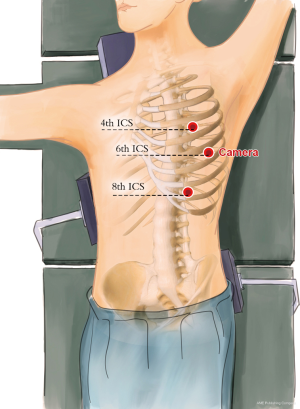
For the left Da Vinci surgical robotic approach, the patient was placed in a 45° right lateral decubitus position, with sponge pads placed along the left scapula and behind the patient’s hip. The arm of the patient was positioned parallel to the trunk, allowing for free access to the mid axillary line (Figure 2).
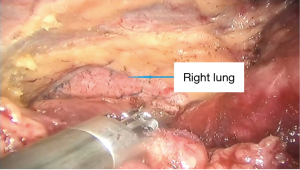
The camera port was made in the 6th intercostal space in the mid-axillary line. Then, the camera was inserted to explore the chest cavity and safely performed the other port incisions. The port for the left robotic arm was subsequently introduced under direct vision in the 8th intercostal space at the anterior axillary line, and the port of right arm was created in the 4th intercostal space at the mid axillary line (Figure 3).
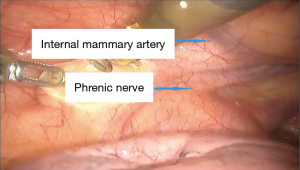
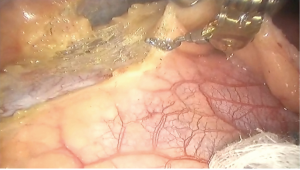
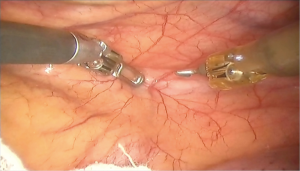
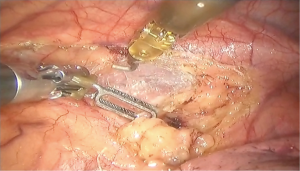
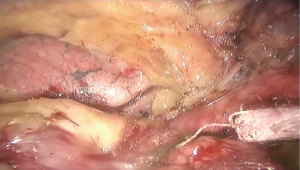
For the left arm, which was mainly used to grasp the adjacent tissue of the tumor, an Endo-Wrist instrument was used, and for the right arm, which was used to perform the dissection, an Endo-hook device with electric cautery function was mainly used (Figures 4,5,6,7,8,8,9,10,11).

After irrigation with warm saline solution, a 32F drainage tube was placed through the incision of the 8th intercostal space. The other incisions were closed.
Postoperative outcome
The patient received phlegm-resolving treatments postoperatively, and the thoracic drainage tube was withdrawn on the second day after surgery. The patient was discharged from the hospital on the third day.
Comment
There have been numerous articles on the efficacy of robotic surgery for mediastinal diseases in recent years. The Da Vinci Surgical System offers a clear benefit compared with video-assisted thoracoscopic surgery and in small well-circumscribed tumours, even with an open approach. Because of the three-dimensional, high definition view and better maneuverability and dexterity of the robotic platform, the surgeon is able to perform surgery with high precision (1).
Thymoma patients may have symptoms of myasthenia gravis (MG) during the perioperative period. It is impossible to overstate the importance of a radical thymectomy for the MG patients. The robotic approach allows for a radical thymectomy which could improve the complete remission rate for MG when compared with the conventional thoracoscopic technique (2).
Because a radical thymectomy is achievable from one side only when using a robotic system, choice of the side is a key issue. The anatomic considerations for the distribution of thymic tissue and the surgeon’s preference are the major factors that guide the choice (3-5).
Factors supporting a left-sided approach include thymic tissue extending lateral to or under the left phrenic nerve (6), up to the cardiophrenic area which requires more dissection on the left side, and ectopic thymic tissue in the aortopulmonary window.
The advantage of a right-sided approach include better visualization of the junction between the innominate vein and superior vena cava, better visualization and dissection of the aortocaval groove, and better ergonomic position to accomplish dissection in the caudal-to-cephalad direction from the right side.
If the tumor is located in the middle or the left side of the body, we choose the left side for robotic-assisted thoracoscopic resection of the thymoma. If the tumor is located in the right side of the body, we choose the right side for robotic-assisted thoracoscopic resection of the thymoma. In patients without MG, in whom contralateral pericardial fat cannot be approached, we dissect the perithymic fat.
We have performed more than ten robotic thymectomies without any conversion to median sternotomy or thoracotomy. Unilateral left-sided 3-port approach was used in most patients.
In conclusion, complete resection of thymomas and adjacent tissues with the da Vinci Surgical System is feasible and safe, and the short-term outcomes such as hospital stay and complication rate were favorable.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.01.16). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schneiter D, Tomaszek S, Kestenholz P, et al. Minimally invasive resection of thymomas with the da Vinci® Surgical System. Eur J Cardiothorac Surg 2013;43:288-92. [Crossref] [PubMed]
- Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg 2011;141:673-7. [Crossref] [PubMed]
- Ismail M, Swierzy M, Rückert JC. State of the art of robotic thymectomy. World J Surg 2013;37:2740-6. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Starting a robotic program in general thoracic surgery: why, how, and lessons learned. Ann Thorac Surg 2011;91:1729-36; discussion 1736-7.
- Mack MJ. Video-assisted thoracoscopy thymectomy for myasthenia gravis. Chest Surg Clin N Am 2001;11:389-405. xi-xii. [PubMed]
- Ismail M, Swierzy M, Rückert RI, et al. Robotic thymectomy for myasthenia gravis. Thorac Surg Clin 2014;24:189-95. vi-vii. [Crossref] [PubMed]
Cite this article as: Chen K, Yang S, Guo W, Jin R, Zhang Y, Chen X, Wu H, Du H, Han D, Xiang J, Li H. Robotic-assisted thoracoscopic thymectomy. AME Med J 2017;2:4.