
Inferior dermoglandular flap for central quadrantectomy in non-ptosis breast cancer patients
Breast-conservation therapy (BCT) is now a standard procedure in early breast cancer which is proved to be safe and equivalent to mastectomy (1-3). Many clinical trial data has been published for more than three decades.
Despite the fact that breast conservative surgery is suitable for most of the early breast cancer patients, there are still some limitations in patient selection such as the unfavorable tumor location. The central and medio-cranial breast cancer (no-man’s land) (4) is found 5–20% in all breast cancer and is more challenging in the cosmetic perspective as it may cause cosmetic unsatisfactory (5). Since the central located tumors has been report to have nipple areola complex (NAC) involvement, most of the time NAC resection is also required to achieve good oncologic outcome (6,7). The tumor in this location use to be one of the indication for mastectomy. Recently, the clinical trials have proved that breast conservative surgery in centrally located tumor is similar to those who undergo mastectomy (8). However, in this particular situation, lumpectomy alone with simple closure may cause the deformities of the breast. This highlights the concepts of ‘immediate partial reconstruction’ during the breast conservative surgery to be able to prevent the poor cosmetic sequelae (9).
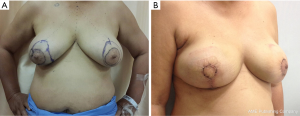
Oncoplastic technique plays an important role in managing central located breast cancer since it gives the opportunity for wider surgical resection which leads to adequate margins and good oncological outcome while maintaining great cosmetic results and patient satisfaction (10). Several procedures have been described to overcome this problem (11-16). However, the most popular and might be the first technique to be described in literature was the Grisotti’s inferior dermoglandular flap. This technique was described by Galimberti et al. (16) and was derived from the reductive mammoplasty technique which base on the inferolateral glandular flap rotation and the skin island that replace the nipple areolar complex. This was proved to be useful and suitable for larger and ptotic breast (Figure 1A,B). However, in our experience, we adapt this technique to suit in non-ptosis moderated sized breast as well. In this study, we describe the case with retroareolar breast cancer in non ptotic breast. The patient underwent central quadrantectomy with sentinel lymph node biopsy. Reshaping the breast by using the vertical skin pattern technique with inferior dermoglandular flap is required to fill the defect after removing central volume of the breast from breast conservative surgery (BCS).
Preoperative evaluation and surgical planning
All patients underwent a physical examination preoperatively and postoperatively. The midsternal and midclavicular lines were marked before surgery as well as the inframammary folds with the patient in the standing position. These anatomical landmarks help the surgeon to define the ideal NAC position. The new NAC location was marked on the breast. The new position of NAC was planned to be 18 to 22 cm from the suprasternal notch. The medial and lateral incision were created by displacing the breast to superolateral and superomedial respectively and draw the line to connect from the dome shape area to the point where meridian line crossed with inframammary fold. This new NAC location was designed beneath the level of the ipsilateral NAC position with the patient’s arm at her side.
Operative technique
With the patient standing, the new NAC area was marked corresponding to the size of the existing NAC (Figure 2A). The skin area was carefully deepithelialized with a number-10 blade (Figure 2B), preserving the complete thickness of the dermis layer. The glandular breast tissue was routinely dissected very close to the dermis and 3 cm around the incision. This makes it possible to mobilize the flap upward to replace the old nipple areolar complex (Figure 2C). Central quadrantectomy with NAC removal was performed through a cutaneous incision located above the tumor site (Figure 2D). The patient was moved to a seated position and the new NAC location was determined. The skin island was then placed on the de-epithelialized bed (Figure 2E,F) and fixed with interrupted subcuticular 4-0 poliglecaprone suture around the edge of NAC area (Figure 2G). The patients were followed at the outpatient department and the inferior dermoglandular flap was examined on postoperative day 7 to 14 (Figure 2H,I).

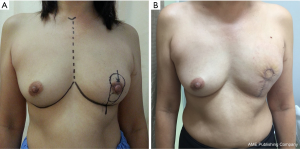
A major disadvantage of our technique is the high-riding of the new NAC location (17) (Figure 3A,B) that can prevent by narrowing the vertical incision with limitation of skin removal above the original NAC.
In conclusion, a simple and effective technique of the inferior dermoglandular flap is presented, in combination with the vertical skin pattern. This combined method allows correction of the central located tumor and parenchyma defect after BCS in all cases with acceptable results.
Acknowledgements
We wish to acknowledge our clinical fellows team as follows: Dr. Saowanee Kitudomrat, Dr. Paweena Luadthai, Dr. Surakit Pornchai and Dr. Watoo Vassanasiri to encourage this operation.
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.02.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Veronesi U, Cascinelli N, Mariani L, Greco M, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [Crossref] [PubMed]
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [Crossref] [PubMed]
- Simone NL, Dan T, Shih J, et al. Twenty-five year results of the national cancer institute randomized breast conservation trial. Breast Cancer Res Treat 2012;132:197-203. [Crossref] [PubMed]
- Fitzal F, Nehrer G, Hoch D, et al. An oncoplastic procedure for central and medio-cranial breast cancer. Eur J Surg Oncol 2007;33:1158-63. [Crossref] [PubMed]
- Foersterling E, Golatta M, Hennigs A, et al. Predictors of early poor aesthetic outcome after breast-conserving surgery in patients with breast cancer: initial results of a prospective cohort study at a single institution. J Surg Oncol 2014;110:801-6. [Crossref] [PubMed]
- Wang J, Xiao X, Wang J, et al. Predictors of nipple-areolar complex involvement by breast carcinoma: histopathologic analysis of 787 consecutive therapeutic mastectomy specimens. Ann Surg Oncol 2012;19:1174-80. [Crossref] [PubMed]
- Vyas JJ, Chinoy RF, Vaidya JS. Prediction of nipple and areola involvement in breast cancer. Eur J Surg Oncol 1998;24:15-6. [Crossref] [PubMed]
- Wagner E, Schrenk P, Huemer GM, et al. Central quadrantectomy with resection of the nipple-areola complex compared with mastectomy in patients with retroareolar breast cancer. Breast J 2007;13:557-63. [Crossref] [PubMed]
- Clough KB, Cuminet J, Fitoussi A, et al. Cosmetic sequelae after conservative treatment for breast cancer: classification and results of surgical correction. Ann Plast Surg 1998;41:471-81. [Crossref] [PubMed]
- Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 2003;237:26-34. [Crossref] [PubMed]
- Holmes DR, Schooler W, Smith R. Oncoplastic approaches to breast conservation. Int J Breast Cancer 2011;2011:303879. [Crossref] [PubMed]
- Moustafa A, Fakhr I. Outcome of different oncoplastic surgical (OPs) techniques for centrally located breast cancer (CLBC). J Egypt Natl Canc Inst 2014;26:203-9. [Crossref] [PubMed]
- Naguib SF. Oncoplastic resection of retroareolar breast cancer: central quadrantectomy and reconstruction by local skin-glandular flap. J Egypt Natl Canc Inst 2006;18:334-47. [PubMed]
- Della Rovere GQ, Pillarisetti RR, et al. Oncoplastic surgery for retro areolar breast cancer - a technical modification of the Grisotti flap. Indian J Surg 2007;69:160-2. [Crossref] [PubMed]
- White J, Achuthan R, Turton P, et al. Breast conservation surgery: state of the art. Int J Breast Cancer 2011;2011:107981. [Crossref] [PubMed]
- Galimberti V, Zurrida S, Zanini V, et al. Central small size breast cancer: how to overcome the problem of nipple and areola involvement. Eur J Cancer 1993;29A:1093-6. [Crossref] [PubMed]
- Rietjens M, De Lorenzi F, Andrea M, et al. Free nipple graft technique to correct nipple and areola malposition after breast procedures. Plast Reconstr Surg Glob Open 2013;1:e69. [Crossref] [PubMed]
Cite this article as: Chirappapha P, Sukpanich R, Sukarayothin T, Leesombatpaiboon M, Trikunakonvong N, Rattadilok C, Kongdan Y. Inferior dermoglandular flap for central quadrantectomy in non-ptosis breast cancer patients. AME Med J 2017;2:20.

