Global epidemiology and future trends of heart failure
Introduction
Irrespective of the underlying cause, heart failure (HF) generates an enormous clinical, societal and economic burden. Although some population statistics suggested that the epidemiologic burden of HF may have significantly decreased between 2000 and 2010 (1), this trend could not be confirmed in other continental or nationwide surveys, which showed instead that both the incidence and prevalence of HF may be increasing especially due to a constantly growing proportion of population aged 70 years or older (2-5). Accurate assessment of epidemiologic trends is vital for optimizing healthcare resources allocation in a world still plagued by an unprecedented economic crisis (6). Therefore, in this brief report, we aimed to provide an objective and concise analysis of the worldwide epidemiological burden of HF, providing also an estimation of possible future trends.
Methods
An electronic search was performed in the Global Health Data Exchange (GHDx) registry, a large database of health-related data maintained by the Institute for Health Metrics and Evaluation (7), using the keyword “heart failure” [International Classification of Diseases 10 (ICD-10) Code I50] in the category “impairment” combined with “all causes” in the category “cause”. According to the Global Burden of Disease (GBD) Collaborators, HF clinically diagnosed, using structured criteria such as those of Framingham or the European Society of Cardiology (ESC) (8,9). Mild HF was then defined as shortness of breath and fatigue with moderate physical activity such as walking uphill or more than a quarter-mile on level ground (disability weight, 0.041; 95% confidence interval (CI), 0.026–0.062), moderate HF as is shortness of breath and easy fatigue with minimal physical activity such as walking a short distance (disability weight, 0.072; 95% CI, 0.047–0.103), whilst severe HF was defined as shortness of breath and fatigue even at rest (disability weight, 0.179; 95% CI, 0.122–0.251) (10). The years lost due to disability (YLDs) was considered the indicator of disease or risk factor attributable to health loss, reflecting the burden of living with a certain disease or disability. The database search was then combined with the epidemiologic variables “year”, “sex”, “age” and “location” (using “SDI Regions”, where SDI stands for socio-demographic index).
The output of the electronic search was downloaded in comma-separated values (CSV), imported into an Excel file (Microsoft, Redmond, WA, USA) and analyzed with Analyse-it (Analyse-it Software Ltd, Leeds, UK) and MedCalc statistical software (MedCalc Software, Ostend, Belgium). Simple (Pearson’s correlation) regression analyses were used for assessing potential associations (and their relative 95% CI) among different epidemiologic measures, whilst the risk was expressed as odds ratio (OR) and relative 95% CI. The study was performed in accordance with the Declaration of Helsinki and under the terms of relevant local legislation.
Results
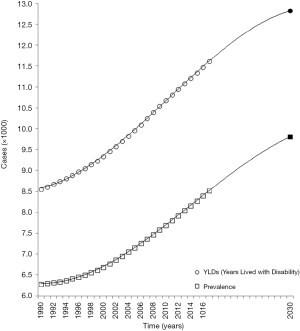
According to the last searchable GDHx period (i.e., year 2017), the current worldwide prevalence of HF is estimated at 64.34 million cases (8.52 per 1,000 inhabitants, 29% of which mild, 19% moderate and 51% severe HF), accounting for 9.91 million YLDS (11.61 per 1,000 YLDs). Based on an American Heart Association (AHA) estimation of 5380 US $ per HF case (11), the current worldwide economic burden of HF can be estimated at 346.17 billion US $. The most frequent causes of HF with known etiology is ischemic heart disease (42.3% of all cases), followed by chronic obstructive pulmonary disease (37.0%), mitral valve disease (4.3%), aortic valve disease (3.4%), rheumatic heart disease (3.0%), myocarditis (2.6%) and endocarditis (1.4%). The last 28-year trend (i.e., between the years 1990 to 2017) is shown in Figure 1. A considerable increase has occurred for both prevalence and YLDs of HF, both trends perfectly matching a third-degree polynomial equation (r=1.000 and P<0.001 for both). Overall, prevalence and YLDs of HF have increased by ~36% since the year 1900, and this trend is not likely to reverse soon. According to estimations based on the third-degree polynomial equations, prevalence and YLDs will probably grow to 9.81 per 1,000 inhabitants (+15.1%) and 12.82 per 1,000 YLDs (+10.4%) by the year 2030, accounting for ~398.44 billion US $ worldwide expenditure.
Although the prevalence of HF appears significantly higher in the female sex (9.16 vs. 7.69 per million inhabitants; OR, 1.19; 95% CI, 1.18–1.20; P<0.001), the value of YLDs is instead marginally but significantly higher in men than in women (11.74 vs. 11.50 per 1,000 YLDs; OR, 1.02; 95% CI, 1.01–1.03; P<0.001). Both prevalence and YLDs have remained almost constant between genders during the last 28 years. The current and last 28-year trend of prevalence and YLDs of HF in different age groups are shown in Figure 2A. Overall, HF poses the largest burden after 60 years of age (81% and 87% of all HF cases and all YLDs for HF, respectively). The risk of developing HF is over 20-fold higher in people aged ≥60 years than in younger subjects (OR: 21.9; 95% CI, 21.8–22.0; P<0.001). Importantly, the prevalence and YLDs of HF have increased by 3.9% and 4.5% in very elderly people (i.e., aged ≥80 years) during the last 28 years. The burden of HF in the different SDI areas is finally shown in Figure 2B. A linear, direct relationship can be found between SDI and both prevalence (r=0.94, 95% CI, 0.31–1.00; P=0.019) or YLDs (r=0.92; 95% CI, 0.20–0.99; P=0.027) of HF.
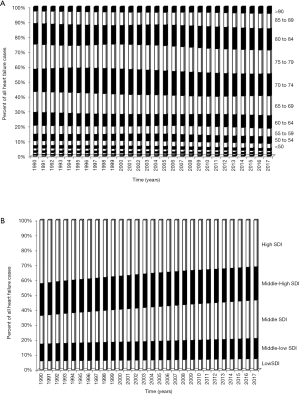
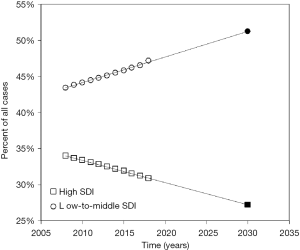
Though the burden of HF remains higher in high SDI regions (31% of all HF cases and 28% of all YLDs for HF), the 28-year trends reveal a −11.2% decreased prevalence in these regions counterbalanced by a 10.3% increase in low-to-middle SDI regions. The YLDs trend is very similar, with a 10.5% decline in high SDI regions occurred during the last 28 years, counterbalanced by a 10.0% increment in low-to-middle SDI regions. The last 10-year trend of HF prevalence seems virtually linear both in high SDI (r=0.999; P<0.001) and low-to-middle SDI (r=1.000; P<0.001) regions (Figure 3). By the year 2030, it can hence be estimated that the prevalence of HF will increase over 50% in low-to-middle SDI regions, whilst it will decline to ~27% in high SDI countries, respectively.
Discussion
Although evidence has been provided that the epidemiologic impact of HF may have decreased during the past decades (1), more recently published continental or nationwide studies showed an almost opposite trend (2-5). The results of our analysis suggest that both prevalence and health loss (i.e., YLDs) of HF have constantly increased during the past 28 years on a worldwide scale, following a path that is unlikely to reverse in the next 10 years based on our estimations. The recent AHA projections show that the prevalence of HF in the US will probably increase from 2.42% in 2012 to 2.97% in 2030 (11), exhibiting a relative increment of 22.7% that would perfectly overlap the increment of worldwide prevalence predicted by our estimation during the same period of time (7.93 per 1,000 inhabitants in 2012 vs. 9.81 per 100 inhabitants in 2030, +23.7%) (Figure 1). Notably, this increased population burden will then translate into an enhanced worldwide expenditure for managing HF patients, which will reach approximately 400 billion US $ in 2030, thus approximating the gross domestic product of an entire country like Austria, Ireland or Israel. Although the sex distribution of HF has not apparently changed during the last 28 years, with prevalence constantly higher in the female sex and YLDs slightly larger in men, the impact of HF in different age ranges has instead significantly varied, with an ~4% increase in the very elderly population, as possible reflection of worldwide population ageing. This increment has been almost constant and has even sharpened during the last 10 years (+ ~2%; Figure 2A), which would hence lead us to estimate that both prevalence and YLDs will consistently increase over 30% in people aged ≥80 years by the year 2030. Since the higher inpatient costs for managing HF are those resulting from hospital readmissions (12), which are up to 4-fold higher in the elderly (13), it is hence very likely that the epidemic proportion reached by HF in older individuals may consistently amplify the usage of healthcare resource for managing HF in the next 10 years.
The last 28-year trend and the current socioeconomic distribution of HF around the world deserve special focus. Although the burden of HF is still largely prevalent in middle-to-high SDI regions, the recent trend shows that the distribution may soon change (Figure 2B). More specifically, our analysis shows that the burden of HF has increased by 3.1% in the last 10 years in low-to-middle SDI regions (from 43.4% to 46.5% of all worldwide HF cases), which would allow us to estimate that the burden of this condition will overcome 50% by the year 2030, thus reversing the current scenario where HF is more prevalent in middle-to-high SDI countries (Figure 3). This prediction will pose additional challenges, whereby HF in low-income countries is clinically different from Europe and North America and its outcome is dramatically influenced by worse health-care infrastructure availability, as well as by lower care access and quality (14). This will require definition and implementation of highly tailored healthcare measures that may pose a theoretically unsustainable burden on local healthcare systems in these countries (15).
Conclusions
The results of our analysis attest that HF is an emerging worldwide threat whose prevalence and health loss burden are constantly increasing, especially in the elderly and in people leaving in low SDI regions. Urgent interventions shall hence be prioritized and scaled up for targeting the cause of HF and preventing its onset and worsening, as well as for redesigning healthcare access, infrastructure and therapies around this evolving epidemiology.
Acknowledgments
Funding: Fabian Sanchis-Gomar is supported by a postdoctoral contract granted by “Subprograma Atracció de Talent - Contractes Postdoctorals de la Universitat de València”.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj.2020.03.03/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med 2015;175:996-1004. [Crossref] [PubMed]
- Guha K, McDonagh T. Heart failure epidemiology: European perspective. Curr Cardiol Rev 2013;9:123-7. [Crossref] [PubMed]
- Roth GA, Forouzanfar MH, Moran AE, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med 2015;372:1333-41. [Crossref] [PubMed]
- Conrad N, Judge A, Tran J, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 2018;391:572-80. [Crossref] [PubMed]
- Cleland JGF, van Veldhuisen DJ, Ponikowski P. The year in cardiology 2018: heart failure. Eur Heart J 2019;40:651-61. [Crossref] [PubMed]
- Krech R, Kickbusch I, Franz C, et al. Banking for health: the role of financial sector actors in investing in global health. BMJ Glob Health 2018;3:e000597. [Crossref] [PubMed]
- Institute for Health Metrics and Evaluation. Global Health Data Exchange. Available online: http://ghdx.healthdata.org/gbd-results-tool. Accessed August 7 2019.
- The Framingham Study. Criteria For Events. Available online: http://www.framinghamheartstudy.org/share/protocols/soe0_03s_protocol.pdf. Accessed August 12 2019.
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129-200. [Crossref] [PubMed]
- Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858. [Crossref] [PubMed]
- Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019;139:e56-e528. [Crossref] [PubMed]
- Lesyuk W, Kriza C, Kolominsky-Rabas P. Cost-of-illness studies in heart failure: a systematic review 2004-2016. BMC Cardiovasc Disord 2018;18:74. [Crossref] [PubMed]
- Akintoye E, Briasoulis A, Egbe A, et al. National Trends in Admission and In-Hospital Mortality of Patients With Heart Failure in the United States (2001-2014). J Am Heart Assoc 2017; [Crossref] [PubMed]
- Dokainish H, Teo K, Zhu J, et al. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet Glob Health 2017;5:e665-72. [Crossref] [PubMed]
- Maggioni AP. Uncovering difference: a glimpse at patients with heart failure in low-income and middle-income countries. Lancet Glob Health 2017;5:e634-5. [Crossref] [PubMed]
Cite this article as: Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J 2020;5:15.