Robotic thoracic surgery: left inferior lobectomy
Clinical data
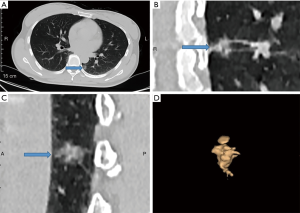
The patient was a 44-year-old woman admitted because of a pulmonary nodule detected by computed tomography (CT). She had seen a doctor because of chest pain 2 weeks previously. Chest CT scan revealed a nodule located in the left lower lobe. The patient had no other symptoms, such as cough, fever, or dyspnea. Three-dimensional (3D) reconstruction of the pulmonary nodules with high-resolution CT showed a mixed density nodules in the left lower lobe of the lung with irregular shape and borders, and spicules, which suggested a malignant lesion. There was no positive sign or supraclavicular lymph node enlargement on physical examination. The patient’s cardiopulmonary function, blood gas analysis, and laboratory tests were normal. She had no medical history. Preoperative stage was cT1N0M0 (IA). The preoperative data suggested a malignant tumor in the left lower lobe of the lung; therefore, the left inferior lobectomy was performed.
Three-dimensional reconstruction CT shows a mixed density nodules on the left lower lobe of the lung (Figure 1). The lesion was irregular in shape, with spiculation, pleural traction, and multiple visible vessels, but no sign of vascular bundles or vacuoles. The plain scan CT value was about −216 Hu. The anteroposterior diameter of the nodule was 18.2 mm, left-right diameter was 14.8 mm, vertical diameter was 14 mm, and volume was about 507 mm3. The solid part was in the center of the lesion, accounting for nearly half of the nodule.
Operation steps
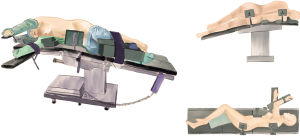
Anesthesia and body position (1)
After the induction of general anesthesia, the patient was placed in a right lateral decubitus position under double-lumen endotracheal intubation with single-lung (right) ventilation. With his hands placed in front of head, the patient was fixed in the jackknife position (Figure 2).
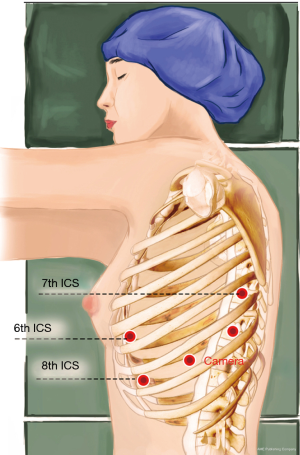
Ports
A 1.5-cm camera port (for a 12-mm trocar) was created in the 8th intercostal space (ICS) at the left mid axillary line, and three separate 1.0-cm working ports (for 8-mm trocars) were made in the 6th ICS (#1 arm) at the left anterior axillary line, the 8th ICS (#2 arm) at the left posterior axillary line, and the left 7th ICS (#3 arm), 2 cm from the spine. An auxiliary port (for a 12-mm trocar) was made in the 8th ICS near the costal arch (Figure 3).
Installation of the surgical arms (1,2)
The robot patient cart is positioned directly above the operating table and then connected. The #2 arm was connected to a bipolar cautery forceps, and the #1 arm was connected to a unipolar cautery hook. An incision protector was used in the auxiliary port.
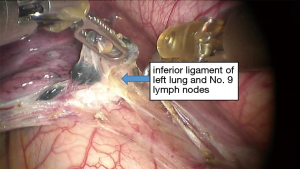
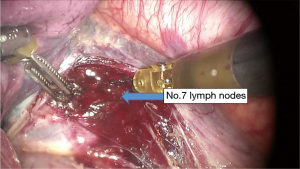
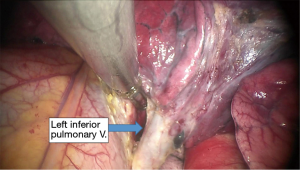
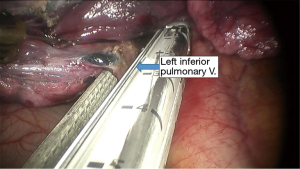
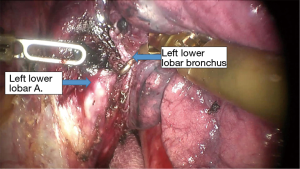
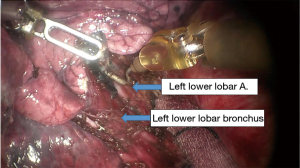
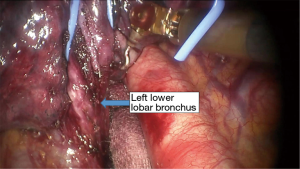
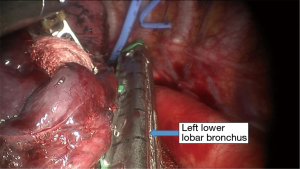
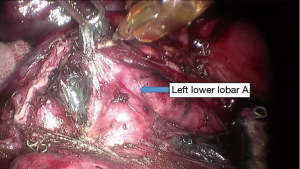
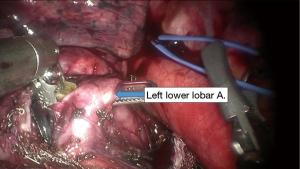
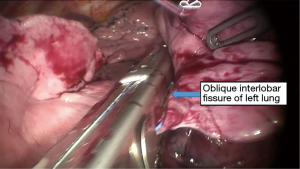
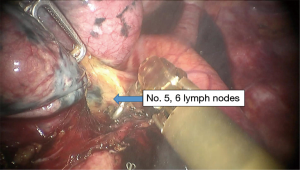
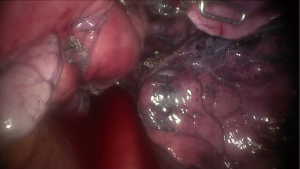
Surgical procedure (1-5)
See Figures 4,5,6,7,8,9,10,11,12,13,14,15,16,17.
Postoperative condition
Postoperative treatments included anti-inflammatory and phlegm-resolving treatment. The thoracic drainage tube was withdrawn 1 day after surgery, and the patient was discharged 3 days after surgery. No complications were observed during hospitalization.
Pathologic diagnosis was invasive adenocarcinoma of the left lower lobe. All lymph nodes were negative. Postoperative pathological stage was pT1N0M0 (stage IA adenocarcinoma).
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.01.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xu S, Meng H, Wang T, et al. Robotic-assisted left inferior lobectomy. Ann Transl Med 2015;3:169. [PubMed]
- Zhao Y, Jiao W, Ren X, et al. Left lower lobe sleeve lobectomy for lung cancer using the Da Vinci surgical system. J Cardiothorac Surg 2016;11:59. [Crossref] [PubMed]
- Augustin F, Bodner J, Wykypiel H, et al. Initial experience with robotic lung lobectomy: report of two different approaches. Surg Endosc 2011;25:108-13. [Crossref] [PubMed]
- Dolezel J, Vlcek P. Robot-assisted pulmonary lobectomy. Bratisl Lek Listy 2008;109:251-3. [PubMed]
- Gharagozloo F, Margolis M, Tempesta B. Robot-assisted thoracoscopic lobectomy for early-stage lung cancer. Ann Thorac Surg 2008;85:1880-5; discussion 1885-6.
Cite this article as: Jin R, Yang S, Guo W, Zhang Y, Chen X, Wu H, Du H, Han D, Chen K, Xiang J, Li H. Robotic thoracic surgery: left inferior lobectomy. AME Med J 2017;2:13.