
An unusual case of esophageal adenocarcinoma presenting with disseminated intravascular coagulation (DIC) as a result of carcinomatosis of the bone marrow
Introduction
Esophageal cancer is an aggressive malignancy with the majority of patients presenting at an advanced stage at the time of diagnosis. The most common sites of metastatic disease include liver, lung, bone, adrenal gland, and pleura (1). The incidence of bone marrow metastasis is exceedingly rare and typically occurs in patients with late stage disease. Diffuse infiltrative involvement of cancer cells into the bone marrow resulting in either disseminated intravascular coagulation (DIC) or microangiopathic hemolytic anemia (MAHA) is known as disseminated carcinomatosis of the bone marrow and confers an extremely poor prognosis (2). Herein we present, to our knowledge, the first case of esophageal adenocarcinoma with the unique presentation of disseminated carcinomatosis of the bone marrow causing DIC.
Case presentation
A 73-year-old previously healthy male with a history of coronary artery disease presented with a two-month history of fatigue, low-grade fevers, and night sweats. The patient also reported easy bruising with minor trauma and a spontaneous subconjunctival hemorrhage that occurred one week prior to admission. On review of symptoms, he endorsed a several month history of progressive dysphagia to solids with associated reflux and a 12-pound unintentional weight loss over one month. He had undergone normal screening colonoscopy 10 years prior. He was a former smoker with less than a 10-pack year history and consumed two alcoholic beverages per day. Physical exam was remarkable for diffuse ecchymosis, including a large ecchymosis in the antecubital fossa at his IV insertion site, with the notable absence of palpable lymphadenopathy.
Initial laboratory tests revealed pancytopenia, including a complete blood count that was notable for white blood cell count of 5.1×109/L, hemoglobin of 7.7 g/dL and platelet count of 20×109/L. A peripheral smear revealed rare circulating blasts with occasional promyelocytes and myelocytes, concerning for acute promyelocytic leukemia (APL). Liver function tests were significant for an elevated alkaline phosphatase of 638 IU/L and a decreased albumin of 3.2 g/dL; his transaminases and bilirubin were normal. Patient was also noted to be in DIC with a prothrombin time of 19.5 seconds, partial thromboplastin time of 43 seconds, INR of 1.68, fibrinogen of 130 mg/dL, and D-dimer of 2,898 ng/mL.
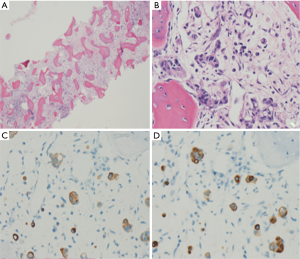
Given high suspicion for APL, the patient was empirically started on all-trans retinoic acid (ATRA). Bone marrow biopsy subsequently demonstrated markedly hypocellular bone marrow (<10%) (Figure 1A) with infiltrative involvement of metastatic adenocarcinoma (Figure 1B). Immunohistochemical testing showed positive staining for CK7 (Figure 1C) and CK20 (Figure 1D), consistent with an upper gastrointestinal primary. Given his reports of progressive dysphagia, upper endoscopy identified a severe, obstructing, and malignant-appearing intrinsic stenosis at the gastroesophageal junction. Biopsies of the stenotic lesion confirmed a moderately differentiated adenocarcinoma with no evidence of HER2 amplification. Tumor marker analysis showed an elevated CA 19-9 of 95.4 U/mL and an elevated CEA of 18 ng/mL. Interestingly, staging CT scans of the chest, abdomen, and pelvis showed no evidence of visceral metastases. There was diffuse heterogeneity of the thoracic and lumbar spine and sternum but no lytic bone lesions. He received supportive care with multiple transfusions of blood products, including packed red blood cells (PRBCs), platelets, fresh frozen plasma (FFP), and cryoprecipitate. He received his first cycle of chemotherapy with 5-fluorouracil (5-FU) with leucovorin and oxaliplatin (FOLFOX) during his initial admission, after which his DIC parameters stabilized and he was discharged home.
He received four cycles of FOLFOX with significant improvement in his platelet count to 85×109/L and hemoglobin to 9.1 g/dL. He did require several PRBC transfusions as an outpatient, and his chemotherapy was delayed after cycle 2 secondary to neutropenia with an absolute neutrophil count of 0.7. His dysphagia improved with no current limitations on oral intake. He subsequently underwent repeat staging that showed progression of disease with new hepatic metastases in addition to widespread osseous metastatic disease, manifesting as new sclerotic and lytic metastases of the lumbar spine, pelvis, and proximal femurs. These findings were not seen on the initial staging scans at the time of diagnosis. Given his preserved performance status, he was initiated on second-line therapy with paclitaxel and the vascular endothelial growth factor receptor (VEGFR) monoclonal antibody ramucirumab.
Discussion
Esophageal cancer, comprised of both squamous cell carcinomas and adenocarcinomas, remains a lethal disease with a high percentage of patients presenting with advanced stages not amenable to surgical cure (3). The majority of patients with stage IV disease present with visceral metastases with only about 5% of patients demonstrating osseous metastases. However, multiple investigators have published reports of a high percentage of bone marrow micrometastases (BMM) in patients with locally advanced esophageal cancer (4-6). A prospective study of patients with esophageal cancer undergoing surgical resection (half of whom received neoadjuvant chemoradiotherapy) found that approximately 50% of patients had BMM at the time of surgery in sampled rib marrow. This study concluded that the detection of BMM is a significant predictor of poor prognosis in patients undergoing resection of esophageal cancer and has been proposed as a means of further staging these patients to predict the risk of developing metastatic disease in the future (7).
While data continues to emerge on the clinical significance of BMM, there is very scant data on the incidence and treatment of diffuse infiltrative bone marrow metastases in esophageal carcinoma. A search of the literature reveals only one other case of esophageal carcinoma with diffuse bone marrow metastasis (8). Two additional case reports and one additional case series have been published on diffuse bone marrow involvement in gastric cancer patients with the overarching theme of limited life expectancies and poor prognoses in these rare patients (9-11). Unlike in our case, however, these patients did not present with or develop DIC.
With disseminated carcinomatosis of the bone marrow, hematologic complications including DIC and MAHA occur as a result of cancer cells diffusely infiltrating the bone marrow and rapidly proliferating. The association between DIC and solid tumor malignancies is rare, and the incidence of DIC in solid tumors ranges from 6.8–15% (12,13). In addition to DIC or MAHA, other biochemical findings of disseminated carcinomatosis of the bone marrow can include severe anemia and a significant elevation in alkaline phosphatase and LDH. Adenocarcinoma is the most common histologic diagnosis when cancer cells invade the bone marrow (14). Among adenocarcinomas, breast, gastric, prostate, and lung are the most frequent primary cancers that may lead to disseminated carcinomatosis of the bone marrow (15-17). There are also rare case reports of disseminated carcinomatosis of the bone marrow occurring in colorectal cancer with a total of 12 reported cases (18).
However, a search of the literature for esophageal cancer associated with disseminated carcinomatosis of the bone marrow yielded no previously reported cases. Therefore, limited data exists to guide the treatment of this patient with chemotherapy drugs that are typically dose reduced or held for cytopenias in the palliative setting to prevent the need for transfusions and growth factor support and to avoid life-threatening infections. One retrospective study of 21 patients with gastric cancer presenting with DIC found that overall survival rates were significantly longer in patients who received palliative chemotherapy as compared to best supportive care (99 vs. 16 days, P<0.001), but the precise chemotherapy regimens varied depending on patient profile, clinical response, and toxicities (1). While our patient did not respond radiographically to first line therapy (as was documented with new liver metastases on serial scans), his cell counts and DIC did stabilize after chemotherapy was initiated with few delays in therapy.
Conclusions
This case is the first described report of esophageal cancer associated with disseminated carcinomatosis of the bone marrow leading to DIC. Despite initiating chemotherapy with less than ideal cell counts, the patient was able to successfully receive months of palliative treatment with an improvement in both his coagulopathy and his dysphagia. We believe that treatment of this unique population should focus on intensive supportive care of DIC as well as consideration of early initiation of chemotherapy.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.02.12). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Quint LE, Hepburn LM, Francis IR, et al. Incidence and distribution of distant metastases from newly diagnosed esophageal carcinoma. Cancer 1995;76:1120-5. [Crossref] [PubMed]
- Rhee J, Han SW, Oh DY, et al. Clinicopathologic features and clinical outcomes of gastric cancer that initially presents with disseminated intravascular coagulation: a retrospective study. J Gastroenterol Hepatol 2010;25:1537-42. [Crossref] [PubMed]
- Lordick F, Mariette C, Haustermans K, et al. Oesophageal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2016;27:v50-v57. [Crossref] [PubMed]
- Ryan P, McCarthy S, Kelly J, et al. Prevalence of bone marrow micrometastases in esophagogastric cancer patients with and without neoadjuvant chemoradiotherapy. J Surg Res 2004;117:121-6. [Crossref] [PubMed]
- Bonavina L, Soligo D, Quirici N, et al. Bone marrow-disseminated tumor cells in patients with carcinoma of the esophagus or cardia. Surgery 2001;129:15-22. [Crossref] [PubMed]
- O'sullivan GC, Sheehan D, Clarke A, et al. Micrometastases in esophagogastric cancer: high detection rate in resected rib segments. Gastroenterology 1999;116:543-8. [Crossref] [PubMed]
- Ryan P, Furlong H, Murphy CG, et al. Prognostic significance of prospectively detected bone marrow micrometastases in esophagogastric cancer: 10-year follow-up confirms prognostic significance. Cancer Med 2015;4:1281-8. [Crossref] [PubMed]
- Chen YH, Huang CH. Esophageal squamous cell carcinoma with dural and bone marrow metastases. World J Gastroenterol 2014;20:12691-5. [Crossref] [PubMed]
- Dittus C, Mathew H, Malek A, et al. Bone marrow infiltration as the initial presentation of gastric signet ring cell adenocarcinoma. J Gastrointest Oncol 2014;5:E113-6. [PubMed]
- Kaur H, Sasapu A, Ramos J, et al. An Unusual Case of Gastric Cancer with Bone Marrow Metastases and Embolic Phenomena as Initial Presentation. J Gastrointest Cancer 2015;46:413-6. [Crossref] [PubMed]
- Ekinci AŞ, Bal O, Ozatlı T, et al. Gastric carcinoma with bone marrow metastasis: a case series. J Gastric Cancer 2014;14:54-7. [Crossref] [PubMed]
- Colman RW, Rubin RN. Disseminated intravascular coagulation due to malignancy. Semin Oncol 1990;17:172-86. [PubMed]
- Sallah S, Wan JY, Nguyen NP, et al. Disseminated intravascular coagulation in solid tumors: clinical and pathologic study. Thromb Haemost 2001;86:828-33. [PubMed]
- Ozkalemkas F, Ali R, Ozkocaman V, Ozcelik T, et al. The bone marrow aspirate and biopsy in the diagnosis of unsuspected nonhematologic malignancy: a clinical study of 19 cases. BMC Cancer 2005;5:144. [Crossref] [PubMed]
- Singh G, Krause JR, Breitfeld V. Bone marrow examination: for metastatic tumor: aspirate and biopsy. Cancer 1977;40:2317-21. [Crossref] [PubMed]
- Ringenberg QS, Doll DC, Yarbro JW, et al. Tumors of unknown origin in the bone marrow. Arch Intern Med 1986;146:2027-8. [Crossref] [PubMed]
- Kucukzeybek BB, Calli AO, Kucukzeybek Y, et al. The prognostic significance of bone marrow metastases: evaluation of 58 cases. Indian J Pathol Microbiol 2014;57:396-9. [Crossref] [PubMed]
- Nakashima Y, Takeishi K, Guntani A, et al. Rectal cancer with disseminated carcinomatosis of the bone marrow: report of a case. Int Surg 2014;99:518-22. [Crossref] [PubMed]
Cite this article as: Raybould AL, Rollins-Raval MA, McRee AJ. An unusual case of esophageal adenocarcinoma presenting with disseminated intravascular coagulation (DIC) as a result of carcinomatosis of the bone marrow. AME Med J 2017;2:25.

