Acetaminophen induced acute liver failure with improving liver biochemistry but worsening cerebral edema: when the king’s college criteria do not help you
Introduction
Although acetaminophen induced liver failure requiring liver transplantation should be rare when treated early with N-Acetylcysteine, it is still one of the most common causes of acute liver failure in the United States and Canada (1,2). The King’s College Criteria (ref: cite ref from PubMed) was developed to assess prognosis of acetaminophen and non-acetaminophen induced liver failure. There is paucity of evidence for the management and natural history of acute liver failure if the biochemical picture does not meet the criteria and even start to improve but imaging, as well as clinical neurological status, shows progression of cerebral edema. Wither watchful waiting will lead to eventual recovery of cerebral edema or to the catastrophic progression to brainstem herniation is not known. There is no literature or scoring system to risk stratify such patients.
Case presentation
A 32-year-old Caucasian man presented to the Emergency Department, and was transferred to our hospital, after ingestion of around 20 g of acetaminophen. The patient did not have any psychiatric history but was going through a stressful relationship event. When he presented 3 days later, he was found to be jaundiced and mildly confused but conversant. Examination was significant for asterixis but no evidence or any stigmata of chronic liver disease. Laboratory evaluation showed acute kidney injury, elevated liver tests and coagulopathy (Table 1). Ultrasound of the liver was unremarkable and laboratory tests for other causes of liver disease including viral hepatitis (i.e., hepatitis A to E), ceruloplasmin and autoimmune hepatitis serology were negative.
Table 1
| Test | Presentation | 48 h later |
|---|---|---|
| GGT (U/L) | 162 | 93 |
| ALP (U/L) | 142 | 99 |
| Bilirubin (μmol/L) | 187 | 87 |
| ALT (U/L) | 6,646 | 2,259 |
| AST (U/L) | 1,983 | 213 |
| Albumin (g/L) | 32 | 23 |
| LDH (U/L) | 476 | 340 |
| Creatinine (μmol/L) | 818 | 354 |
| INR | 4.4 | 1.9 |
| PTT (s) | 26 | 27 |
| Lactate (mmol/L) | 3 | 2.6 |
| Arterial PH | 7.4 | 7.4 |
Note the marked improvement at 48 h. GGT, gamma-glutamyl transferase; ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; LDH, lactate dehydrogenase; INR, international normalized ratio; PTT, partial thromboplastin time; PH, potential of hydrogen.
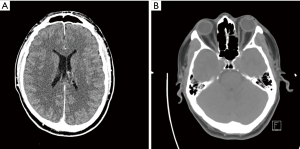
The patient was admitted to the intensive care unit for supportive management and N-acetylcysteine infusion was started. Unfortunately, his level of consciousness deteriorated and had an episode of tonic clonic seizures. An urgent CT scan of the head showed diffuse cerebral edema (Figure 1) and the patient was started on Hypertonic saline and Mannitol. After 24 hours, blood tests showed significant improvement (Table 1) but CT scan showed worsening of cerebral edema and the patient remained intubated, mechanically ventilated with no improvement in neurological status as well as sluggish pupillary reflexes (Figure 2).
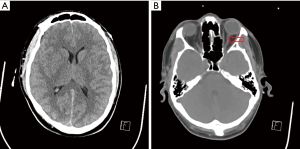
The worsening cerebral edema and neurological function was concerning despite the improvement in liver biochemistry. A liver organ suddenly became available and after a multidisciplinary discussion with hepatobiliary surgery, the ICU staff, Psychology, Social worker, and the patient’s family. It was decided to proceed with orthotropic liver transplantation given the uncertainty regarding the worsening neurological status and cerebral edema on imaging. Post-transplant, the patient made an excellent recovery with rapid neurological and cognitive improvement and he was discharged from hospital 2 weeks later. His post-transplant course was complicated by mild acute cellular rejection which was treated with pulse corticosteroids.
The explanted liver histology showed massive hepatic necrosis with no evidence of fibrosis or necroinflammation, consistent with acute acetaminophen toxicity.
Discussion
We present a rare case of a challenging situation. It was not clear if the patient’s cerebral edema would improve despite his improving liver parameters and there was a risk of cerebral herniation which would have been a fatal complication. From a biochemical perspective, the patient did not meet the King’s College criteria for liver transplantation and it could be questioned whether liver transplantation was appropriate. We note that a systematic review has reported that the sensitivity and specificity of King’s College criteria is 57% and 95% respectively (4) but that is not in the setting of worsening cerebral edema. It is thought that grade IV hepatic encephalopathy is associated with less than 20% chance of spontaneous recovery (5). It was decided after a multidisciplinary team discussion that proceeding with liver transplant impose less risk than continue conservative management, especially with the patient’s worsening neurological status. There is no tool or criteria to guide or predict the course of cerebral edema in this setting. In our search, we found no reported cases with such course. More studies are needed to determine the natural history of cerebral edema in the setting of improving laboratory parameters. This is important for resource allocation and to avoid life-long immunosuppression and the potential complications of liver transplantation.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.06.02). Eric M. Yoshida serves as an unpaid board member of AME Medical Journal from Jun 2017 to Jun 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ostapowicz G, Fontana RJ, Schiødt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002;137:947-54. [Crossref] [PubMed]
- Gill RQ, Sterling RK. Acute liver failure. J Clin Gastroenterol 2001;33:191-8. [Crossref] [PubMed]
- Tso MO, Hayreh SS. Optic disc edema in raised intracranial pressure. IV. Axoplasmic transport in experimental papilledema. Arch Ophthalmol 1977;95:1458-62. [Crossref] [PubMed]
- Craig DG, Ford AC, Hayes PC, et al. Systematic review: prognostic tests of paracetamol-induced acute liver failure. Aliment Pharmacol Ther 2010;31:1064-76. [PubMed]
- O'Grady JG, Alexander GJ, Hayllar KM, et al. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 1989;97:439-45. [Crossref] [PubMed]
Cite this article as: Kayal A, Marquez-Azalgara V, Erb SR, Scudamore CH, Yoshida EM. Acetaminophen induced acute liver failure with improving liver biochemistry but worsening cerebral edema: when the king’s college criteria do not help you. AME Med J 2017;2:73.