
For “time is the brain”, what can be done prehospital
Ischemic stroke is one of the leading causes of death or permanent disability. Based on several prospective randomized trials, administering intravenous recombinant tissue plasminogen activator (tPA) within 4.5 h or intraarterial treatment (IAT) within 8 h of acute ischemic stroke (AIS) onset may reduce the disability risk (1,2). However, before the tPA therapy or IAT given, complicated diagnosis to exclude hemorrhage or other therapies contraindications are required. The diagnosis includes: neurological examination, radiological and laboratory tests (3). Time from symptom onset to treatment initiation has a close relationship with the success. But in actual clinical practice, it is difficult to ensure that AIS patients can get treatment within the time window.
To reduce the delay, many methods have been established for fast prehospital treatment (3). In this review, we describe the importance of time for acute stroke therapy, analyze the possible causes of time delay, present the main methods of saving time in the clinic, and analyze the problems of these methods.
The importance of time to AIS
As many as 14 billion synapses and 1.9 million neurons may die in each minute a stroke onset but untreated (4). The concept of “time is brain” has been supported by earlier experimental animal research, and is also derived from many observations. Benefit of tPA diminishes with increasing treatment delay. The guidance recommends the routine use of tPA within 4.5 h of stroke onset in Europe. But the Food and Drug Administration (FDA) of USA, approved the use of tPA only within 3 h of stroke onset (5).
A study in 2004 analyzed common data elements from six intravenous tPA randomized trials. By multivariable logistic regression analysis, the researchers assessed the relation of the interval from stroke onset to start of treatment (OTT) on favourable outcome after 3 months. Results showed that Odds of a 3-month outcome increased as OTT decreased (P=0.005). Odds were 1.2 (95% CI, 0.9–1.5) for 271–360 min, 1.4 (95% CI, 1.1–1.9) for 181–270 min, 1.6 (95% CI, 1.1–2.2) for 91–180 min, and 2.8 (95% CI, 1.8–4.5) for 0–90 min in the tPA group (6). The meta-analysis results provided clear evidence for improved odds of a good stroke outcome when treatment is started within 4.5 h of ischemic stroke. Earlier treatment resulted absolute benefits and bigger proportional (7).
If tPA treatment is started within 1.5 h, number needed to treat (NNT) to achieve a good outcome is 4.5. If started within 1.5 to 3 h, NNT double to 9. If treatment initiated within 3.0–4.5 h, NNT is 14.1 (6,8). Fast reperfusion also leads to improved functional outcome among AIS patients with endovascular treatment. In the stent retriever arm of a study, patient’s functional independence probability would get to 91%, if the brain reperfusion resumed at 150 min after stroke symptom onset. Subsequently, the probability was reduced by 20% for each 1 h delay (9). Pre-treatment delay was associated with higher odds of hospital mortality, symptomatic bleeding and lower odds of good outcome after adjusting for patient and hospital characteristics (10).
The time patients need to reach the doors of the hospital is the main reason for treatment delays. Data from the American Get with the Guidelines Stroke Registry in recent years clearly shows that the delays in the time to hospital admission did not improve in recent years. In Germany, the median prehospital time is 151 min, and only 45% of patients can be transferred to the hospital within 3 h (11).
But many problems still existed in the progress of AIS treatment. Continuous public awareness campaigns, personnel emergency medical service education, effective stroke symptom identification scales used, classification to appropriate institutions, and advance notice of receiving hospitals could contribute to more efficient use of resources and reduce the time taken to instigate treatment to within the golden hour of the onset of the symptoms of stroke (5).
Public awareness of stroke
It is helpful to reduce stroke death and disability by recognizing stroke symptoms and acting quickly. But public awareness of stroke risk factors, stroke symptoms and stroke early treatments is still limited. Before 2008, about 24% to 55% of acute stroke patients or their family do not call the emergency medical services (EMS) within 1 h (12). Some relatives of the patients choose a private vehicle to transport the patient to the hospital, but do not notify anyone other. In recent years, data from the American clearly show that, despite considerable attempts to improve public education programs, delays in the time to hospital admission did not ameliorate in recent years.
To solve this problem, educational campaigns are promoted to improve the patients and relatives’ awareness of the correct response to the symptom of stroke (13). Such campaigns have been shown to have a short-term impact on stroke symptom knowledge (14). A recent study interviewed stroke patients, stroke witnesses and primary care clinicians, in order to examine campaign Act FAST (facial droop, arm weakness, speech disturbance, time to call 119) (Figure 1) on stroke awareness and perspectives. Most patients and witnesses felt that the activity affected their identification and response to stroke, but some people thought that the campaign was ineffective (15).

In March 2012, to improve knowledge of stroke symptoms and treatment, Japan government sponsored an educational campaign based on a television commercial. After the education, results showed that in the intervention group, the mean prehospital delay was shorter (12.0 vs. 13.5 h; P=0.0067), the proportion of patients arriving within 3 h was larger (55.7% vs. 46.5%; P=0.0021), and the proportion arriving after 6 h was smaller (32.7% vs. 39.5%; P=0.0162) (16).
Testing is also a common way of stroke knowledge education. To develop an educational program which can improve stroke knowledge and accurate identification of acute stroke within 3 h of symptom onset, a total of 33 providers received a written test about stroke knowledge, diagnosis, and management before, immediately after, and 3 months after. The mean test score improved significantly immediately after the program and lasted 3 months. The linear regression model showed that the scores improved notable, and was not significantly associated with age, gender, working hours and learning or work experience (17).
At present, only a handful of existing studies have analyzed the impact of public awareness campaigns on clinically relevant stroke outcomes (18-23) (Table 1). A review included 22 intervention studies showed that in terms of women preference or type of information retained or media preferred, most interventions proved partially effective. If there is sufficient financial support, the mass media campaigns may be effective. But the role of the mass media movement for high-risk subgroups (aging, linguistic or socioeconomic) is unclear. Although web-based campaigns can effectively attract a large number of people to watch and study the stroke prevention knowledge, but it may not attract the people who often have a certain specificity. Most of these studies reveal the effects of exercise on patient behavior; however, these effects may persist for no more than 5 months (24). Studies have shown that the impact of this campaigns on patients and their families is fairly short-lived, and that constant message repetition is the key to the success.
Table 1
| Author | Year | Site | Study design | Study duration | Number of stroke patients with and without intervention | Time before admission with and without intervention | Thrombolysis rates with and without intervention |
|---|---|---|---|---|---|---|---|
| Alberts et al. | 1992 | Durham, United States | Observational | 3 years | 189 vs. 290 | 86% vs. 37%, P<0.00001 (within 24 h) | N/A |
| Barsan et al. | 1994 | United States | Observational | 3 years | 487 vs. 487 | 1.5 vs. 3.2 h (means, P<0.05) | N/A |
| Morgenstern et al. | 2002 | Texas, United States | Observational | 15 months | 400 vs. 218 (interventional region); 365 vs. 206 (control region) |
36.5% vs. 26.5%, P<0.05 (interventional region, within 2 h); 30.4% vs. 21.4%, P=0.07 (control region, within 2 h) |
5.8% vs. 1.4%, P<0.05 (the interventional region); 0.6% vs. 0.5%, n. s. (the control region) |
| Behrens et al. | 2002 | Mannheim, Germany | Observational | 3 months | 113 vs. 83 | 3.28 h ±40 min vs. 5.22 h ±84 min (means ± SD, P<0.05) |
10.5% vs. 2%, P<0.01 |
| Wojner-Alexandrov et al. | 2005 | Houston, TX, United States | Observational | 3 years | 1,072 vs. 446 | 62% vs. 58%, P=0.002 (within 2 h) |
Increase in 4/6 centers, decrease in 2/6 |
| Hodgson et al. | 2007 | Ontario, Canada | Observational | 31 months | 12,534 (total) | Continuous increase between 2003 and 2005, R2 =0.60, P<0.001 (within 2.5 h) |
|
| Addo et al. | 2012 | London, UK | Observational | 2 years | 154 vs. 195 | 44.9% vs. 40.7% (within 3 h), | 16.4% vs. 16.9% |
N/A, not applicable.
Stroke education should be targeted to special crowd
Findings suggest that public education for stroke is necessary, and stroke education should be more targeted to specific target groups. These groups include elderly, minorities, neighbors of stroke survivors, and students. In a study, researchers distributed leaflets with stroke knowledge at the supermarket’s purchase point for the old people. After 3 weeks, questionnaires had designed for stroke knowledge and emergency treatment after stroke. After campaign, the proportion of correct answers for hemiplegia and unilateral numbness and calling EMS increased significantly (25).
Students also need to give stroke education, because they may be future patients, patients’ relatives, or doctors. It is also important that education should be expressed in a simple and clear statement that should be taken in an emergency situation. Using stroke education system, a schoolteacher can conduct the FAST message lesson to junior high school students with a similar outcome as a stroke neurologist. For the meaning of the FAST, the correct answer rate in the neurologist group is 83%, and is 84% in the schoolteacher group (26).
In addition, stroke education should be particularly strong for some people, such as those with lower levels of education and higher risk factors for stroke. A cox regression analysis showed that educational history was not associated with recurrent strokes, but it associated with favorable post stroke survival independently (27). Educational campaigns should target the groups with increased stroke risk. Tobacco smokers should be targeted in particular, and putting health warning labels on the cigarette packs maybe a good method. People with some stroke risk factors, such as heart disease and obesity, are responsive to information about stroke (28). It is necessary for stroke survivors with low socioeconomic status to reinforce formulating specific strategies for care and treatment (29).
To generate sympathetic feeling and to transmit the importance of active treatment, the National Stroke Association’s Faces of Stroke multimedia public awareness campaign need to tell the stories of stroke survivors and caregivers, to presents stroke patients’ emotional. In addition, health behavior scientists have also played an important role in assessing the concept of public behavior change.
Benefits of the EMS
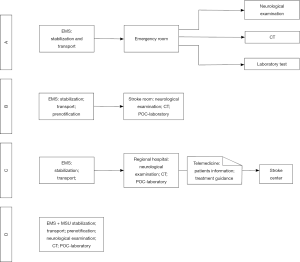
There are different EMS structures in different countries and even within different regions of the country. When the stroke occurs, the role of EMS can be reflected. At present, countries are based on their own national EMS characteristics, developed a corresponding stroke onset plans and guidelines. These guidelines clearly indicate the instruments required to identify the stroke symptoms, the manner of emergency transport, and the indication of the institution (Figure 2).
Studies have shown that the accuracy of the EMS dispatchers accurate identification of stroke is between 30% and 83%, so the further training is necessary (30). Many national and international stroke guidelines have pointed out that, in addition to medical training, there are already many instruments designed to allow the EMS team to assess and identify the occurrence and severity of stroke in the field. Based on the presence of facial paresis, one-sided paresis of an upper extremity, and speech disorder, the Cincinnati Prehospital Stroke Scale is invented. The sensitivity of Cincinnati Prehospital Stroke Scale for the presence of acute stroke is 90%, and the specificity is 66% (31). In addition to the Cincinnati Prehospital Stroke Scale items, the Los Angeles Prehospital Stroke Screen also included four additional questions about history and the results of a glucose test. Although the sensitivity and specificity of Los Angeles Prehospital Stroke Screen are high (91% and 97%), the process is complicated and wasting time (32). FAST stroke assessment is easy to perform and can be used by the general public. Like Cincinnati Prehospital Stroke Scale, the FAST stroke assessment is also based on the presence of facial paresis, one-sided paresis of an upper extremity, and speech disorder. In the FAST evaluation, the importance of time is particularly prominent. This scale system has a sensitivity of 79%, and is so easy to perform that it can even be used by the general public (33).
The transfer of the patient and the transmission of information
It is critical to the outcome of stroke patients for giving stroke patients priority to the stroke centers with experience in stroke therapy and thrombolytic techniques or intravascular treatment techniques. In this way, patients can reduce the delay in treatment and improve the rate of recanalization. If patients are transported to stroke centers rather than to nonspecialized institutions, the treatment rates will increase from 14.1% to 21.9% (OR, 1.72; 95% CI, 1.22–2.43) (34). Even the stroke center is far away from the hospital, patient is still able to get a better prognosis. In order to save the time to the stroke center, some hospitals even use helicopters to transport patients.
When the patient was transferred from the EMS to the hospital, the transmission of information regarding the patient’s symptoms, thrombolytic contraindications and other information to hospital stroke team is critical. Stroke management guidelines additionally recommend prenotification of the receiving hospital about the arriving patient. Through the hospital’s prenotification, the hospital can quickly activate the stroke treatment group and be able to start up computed tomography (CT) early and reduce the treatment delay.
This prenotification allows the fastest possible activation of the stroke team and, especially, the reservation of CT scanners. Previous studies have showed that compared with prenotification of the hospital team alone, in combination with further restructuring of stroke management plans can save the crucial time to therapy and increase thrombolysis rates. Regarding methodology, the transfer of structured clinical data between the EMS team at the emergency site and the hospital stroke team could also be optimized by the use of personal digital assistants or smart phones. In addition, there are many tools that can be used to communicate information between EMS team and the hospital, such as doctors commonly used personal digital assistants and smart phones. The purpose of stroke patient treatment procedures is to do as little as possible after the patient has been arrived in the clinic, and as much as possible when the patient is on the way to the clinic.
For patients who cannot reach the stroke center in a short period of time, system for two-way audiovisual video conferencing and exchange of patient checks and CT scans of video can be used to enable patients to obtain timely treatment of stroke. Previous studies have shown that this telemedicine interaction between the two hospitals is reliable and safe, and that it has a positive impact on thrombolysis rates and clinical outcomes. However, technical problems such as temporary signal loss still hinder the reliable interaction between ambulances and hospitals
Role of mobile stroke unit (MSU)
Following the demonstration that ambulance mounted CT scanners, treatment with tPA can be carried out safely and accurately with a median time between 70 to 80 min. According to the MSU used, shorter time before the treatment is needed, and increased proportion of patients can be treated within the time window. Earlier evaluation and treatment with tPA in the first hour after symptom onset resulted the better outcomes. The absolute number of tPA-treated patients within the 4.5-h window is increased via the MSU (35).
To achieve more stroke patient benefit from recanalization goals, prehospital stroke treatment which is based on the use of an ambulance contains a small CT scanner and a point-of-care laboratory was used. Some ambulances also include devices that allow remote medical care with the hospital, enabling bi-directional communication and transmission of the patient’s video or CT scan from the emergency site to the hospital.
The clinical diagnosis of stroke is based on the presence of a sudden neurological deficit. But without brain imaging, it is not possible to distinguish haemorrhagic and ischaemic stroke. MSU provided the opportunity to integrate small CT scanners into ambulances. This makes it possible for CT imaging to be set up prehospital (Figure 2).
In 2010, Walter et al. from Homburg (Saarland), Germany, first reported the differentiation between ischemic and hemorrhagic stroke was feasible in such a specialized stroke ambulance (36). Ischemic stroke diagnosis was made in a 66-year-old patient after the exclusion of hemorrhage via CT. The diagnosis of hemorrhagic stroke was made in a 63-year-old lady (36). Walter et al. published the results of 53 stroke patients diagnosed in their MSU compared with 47 patients in the control group, in 2012 (3). The time from alarm to end of mobile CT scanning was 34 min (IQR: 30–38 min). In patients with MSU, 55% ischemic strokes and 4% hemorrhagic strokes were diagnosed. In all prehospital cases, stroke mimics were diagnosed in 23% and TIA in 15% (3).
IN the PHANTOM-S study started in 2011, with the remotely read of CT scans via teleradiology, the radiologist is no longer need to on board the ambulance (37). The CT scanner is locked during travel and unlocked when scanning. About 95% of all scans had sufficient quality for reading. The median alarm-to-imaging time after MSU deployment was 35 min. Higher bandwidth of the mobile information technology connection accelerates the transfer images’ quality (38).
As a grading system, Alberta Stroke Program Early CT Score (ASPECTS) is used to assess early ischemic changes on pretreatment CT studies in patients with AIS (39). The neuroradiological expertise of the MSU has been improved by its ability to calculates the electronic-ASPECTS by e-ASPECTS implementation onto the MSU. A study in 2016 illustrated the potential benefits of e-ASPECTS (40). In that study, one patient was directly performed prehospital thrombolysis by excluding early infarct signs. A patient caused by large-vessel occlusion, was decided to initiate intraarterial treatment supported by the high e-ASPECTS value (40). MSU with e-ASPECTS showed that such integration helps to determine the treatment plan and the classification of the most appropriate target hospital.
For the large vessel occlusion, timely endovascular treatment may be more effective on the patients. So MSU with CT scanner enables performance of CT angiography (CTA) of the intracranial vessels, and allows for rapid triage of patients to interventional-capable centers (3,40). A case reported that a patient with new onset of right hemiparesis was teleneurological assessed with a severe left middle cerebral artery (MCA) syndrome. A CTA was performed subsequently confirmed an MCA occlusion. Based on these findings, patient was immediately transferred to the hospital with IAT capability, where he underwent successful recanalization and get an improvement in symptoms (41).
Problems of prehospital stroke treatment
Today, the number of prehospital stroke treatment programs has been growing rapidly in the world. In order to facilitate the exchange of data and strengthen the cooperation, most of these groups cooperate in the context of the Prehospital Stroke Treatment Organization (PRESTO). But there are many reasons directly affects the overall number of patients through prehospital stroke treatment. The reasons include patients living regions and the surrounding environment, regional EMS configuration, and cost-effectiveness. MSU is just one of good strategy for increasing the rate of stroke good outcome. With the constant improvement of the standard prehospital and in-hospital stroke care, good outcome rate of stroke can also be increased significantly. In addition, the public education is also of relevance, because the time from stroke onset to emergency call is beyond the influence of the deployment of an MSU.
At present, there are still some potential problem with earlier treatment on the use of MSU at present. One problem is that the experience of using MSU is not enough in most countries. Studies of MSU were almost finished in European. Stroke centers in other countries do not know how much time can be saved by using MSU. Traffic patterns, distances, local regulations, and care systems are different in different countries. Especially in China, different provinces have distinguishing medical condition features. MSU may be not suitable for some regions of China.
Patients with stroke mimics, such as migraine or seizures, or patients with transient ischemic attacks, have a potential chance of treating on the MSU. In the future, earlier, accurate identification of stroke mimics and appropriate prioritization of patients with true stroke can be an important potential advantage of the MSU concept. To make no different from the rate of stroke mimic treatment with standard management, a physician experienced in stroke treatment should be aboard on the MSU. Because of the difficult of TIA assessed, the TIA incidence could be higher in patients evaluated by MSU. In the National Institute of Neurological Disorders and Stroke (NINDS) study, 2.4% in patients treated 1 to 3 h after symptom onset and 2.1% in patients treated within 1 h completely recovering with 24 h (42). To approximate the percentage of TIA patients in the cohort of tPA treated with MSU, we need to observe patients for whom we do not activate the MSU but meet the criteria for stroke treatment, and then to determine the completely recover proportion of them by the time of tPA decision in the ED.
A third potential problem is that with MSU management, an increase in the number of intracerebral hemorrhages, angioedema, or other complications of tPA treatment will increase. Widely used of the IAT make more patients can achieve recanalization within 4 to 5 h from symptoms onset. Prehospital identification of patients with large artery occlusion, facilitating in-hospital treatment by prehospital notification, earlier assembly of the IAT preparation, and shorter in-house delays incurred by acquiring imaging and laboratory data and treating with tPA might potently reduce time to IAT treatment in MSU.
Cost-effectiveness of prehospital stroke treatment
Evidence shows that as a costly disease, improvements in the process of stroke management, can increase the success rate of thrombolysis, and reduce the overall cost of treatment. In the treatment improvement progress, MSU is criticized because of potentially unacceptable costs. Based published research results of the first trial on MSU concept to one year direct cost savings, Dietrich and colleagues analyzed the incremental direct costs of prehospital stroke treatment (43). The results indicate that based on a 1-year benefit-cost analysis, in a wide range of possible cases, prehospital treatment of acute stroke is highly cost-effective across. If further reduce the staff size of the MSU through telemedical support from hospital experts, the cost-effective can be higher. Even though the efficiency of MSU is positively related to population density, the benefit-cost ratios can be greater than 1 in rural settings. The model of the study implies that in different circumstances, the MSU strategy is cost-efficient starting from a population density of 79 inhabitants per km2 or from an operating distance of 15.98 km.
Gyrd-Hansen and colleagues also has carried on the evaluation to the cost-effectiveness of prehospital stroke treatment. The study registered time to thrombolysis, treatment rates, and all resource consequences of the intervention. According to numbers needed to treat derived from pooled IVT trials and translated Intermediate outcomes, quality-adjusted life years (QALYs) were extrapolated as final outcomes need to gains. Results showed that the net cost of the stroke emergency mobile (STEMO) prehospital stroke concept was euro 963,954 annually. The higher frequency of IVT administrations per year and higher proportions of patients treated in the early time interval resulted in an annual expected health gain of avoidance of 18 cases of disability equaling 29.7 QALYs. Even in health-economic dimensions, depending on willingness-to-pay thresholds in societal perspectives, the STEMO prehospital stroke concept has the potential of providing a reasonable innovation (44).
In summary, this review indicates the importance of prehospital time for AIS, and clarifies some major options that can be implemented for increasing the chances to obtain recanalizing therapy. On the patient’s side, options for the stroke prehospital management include continual public awareness campaigns for target-specific. On the EMS side, stroke symptom recognition tools, prioritized to stroke centers, receiving hospital prenotification, and the used of MSU can shorten the prehospital delay, improve the treatment rates, and even get a cost-effectiveness. In the future, prehospital stroke treatment could be more important for a better stroke management.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.06.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Friedman HS. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1996;334:1405. [Crossref] [PubMed]
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11-20. [Crossref] [PubMed]
- Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol 2012;11:397-404. [Crossref] [PubMed]
- Saver JL. Time is brain - Quantified. Stroke 2006;37:263-6. [Crossref] [PubMed]
- Fassbender K, Balucani C, Walter S, et al. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol 2013;12:585-96. [Crossref] [PubMed]
- Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of Atlantis, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768-74. [Crossref] [PubMed]
- Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929-35. [Crossref] [PubMed]
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317-29. [Crossref] [PubMed]
- Goyal M, Jadhav AP, Bonafe A, et al. Analysis of workflow and time to treatment and the effects on outcome in endovascular treatment of acute ischemic stroke: results from the SWIFT PRIME randomized controlled trial. Radiology 2016;279:888-97. [Crossref] [PubMed]
- Kamal N, Sheng S, Xian Y, et al. Delays in Door-to-Needle Times and Their Impact on Treatment Time and Outcomes in Get With The Guidelines-Stroke. Stroke 2017;48:946-54. [Crossref] [PubMed]
- Rossnagel K, Jungehülsing GJ, Nolte CH, et al. Out-of-hospital delays in patients with acute stroke. Ann Emerg Med 2004;44:476-83. [Crossref] [PubMed]
- Ragoschke-Schumm A, Walter S, Haass A, et al. Translation of the 'time is brain' concept into clinical practice: focus on prehospital stroke management. Int J Stroke 2014;9:333-40. [Crossref] [PubMed]
- Alberts MJ, Perry A, Dawson DV, et al. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke 1992;23:352-6. [Crossref] [PubMed]
- Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, et al. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO) Stroke 2005;36:1512-8. [Crossref] [PubMed]
- Wolters FJ, Paul NL, Li L, et al. Sustained impact of UK FAST-test public education on response to stroke: a population-based time-series study. Int J Stroke 2015;10:1108-14. [Crossref] [PubMed]
- Nishijima H, Kon T, Ueno T, et al. Effect of educational television commercial on pre-hospital delay in patients with ischemic stroke. Neurol Sci 2016;37:105-9. [Crossref] [PubMed]
- Hsieh HC, Hsieh CY, Lin CH, et al. Development of an educational program for staffs of emergency medical service to improve their awareness of stroke within 3 hours of symptom onset: a pilot study. Acta Neurol Taiwan 2013;22:4-12. [PubMed]
- Hodgson C, Lindsay P, Rubini F. Can mass media influence emergency department visits for stroke? Stroke 2007;38:2115-22. [Crossref] [PubMed]
- Morgenstern LB, Staub L, Chan W, et al. Improving delivery of acute stroke therapy: The TLL Temple Foundation Stroke Project. Stroke 2002;33:160-6. [Crossref] [PubMed]
- Barsan WG, Brott TG, Broderick JP, et al. Urgent therapy for acute stroke. Effects of a stroke trial on untreated patients. Stroke 1994;25:2132-7. [Crossref] [PubMed]
- Müller-Nordhorn J, Wegscheider K, Nolte CH, et al. Population-based intervention to reduce prehospital delays in patients with cerebrovascular events. Arch Intern Med 2009;169:1484-90. [Crossref] [PubMed]
- Behrens S, Daffertshofer M, Interthal C, et al. Improvement in stroke quality management by an educational programme. Cerebrovasc Dis 2002;13:262-6. [Crossref] [PubMed]
- Addo J, Ayis S, Leon J, et al. Delay in presentation after an acute stroke in a multiethnic population in South london: the South london stroke register. J Am Heart Assoc 2012;1:e001685. [Crossref] [PubMed]
- Rasura M, Baldereschi M, Di Carlo A, et al. Effectiveness of public stroke educational interventions: a review. Eur J Neurol 2014;21:11-20. [Crossref] [PubMed]
- Inoue Y, Honda S, Watanabe M, et al. Educational campaigns at point of purchase in rural supermarkets improve stroke knowledge. J Stroke Cerebrovasc Dis 2015;24:480-4. [Crossref] [PubMed]
- Miyashita F, Yokota C, Nishimura K, et al. The effectiveness of a stroke educational activity performed by a schoolteacher for Junior high school students. J Stroke Cerebrovasc Dis 2014;23:1385-90. [Crossref] [PubMed]
- Ojala-Oksala J, Jokinen H, Kopsi V, et al. Educational history is an Independent predictor of cognitive deficits and long-term survival in postacute patients with mild to moderate ischemic stroke. Stroke 2012;43:2931-5. [Crossref] [PubMed]
- Sobotková P, Goldemund D, Reif M, et al. Predictors of noticing stroke educational campaign. J Stroke Cerebrovasc Dis 2014;23:1662-8. [Crossref] [PubMed]
- Fernandes TG, Goulart AC, Santos-Junior WR, et al. Educational levels and the functional dependence of ischemic stroke survivors. Cad Saude Publica 2012;28:1581-90. [Crossref] [PubMed]
- Buck BH, Starkman S, Eckstein M, et al. Dispatcher recognition of stroke using the National Academy Medical Priority Dispatch System. Stroke 2009;40:2027-30. [Crossref] [PubMed]
- Kothari RU, Pancioli A, Liu T, et al. Cincinnati prehospital stroke scale: reproducibility and validity. Ann Emerg Med 1999;33:373-8. [Crossref] [PubMed]
- Kim JT, Chung PW, Starkman S, et al. Field validation of the Los Angeles motor scale as a Tool for paramedic assessment of stroke severity. Stroke 2017;48:298-306. [Crossref] [PubMed]
- Harbison J, Massey A, Barnett L, et al. Rapid ambulance protocol for acute stroke. Lancet 1999;353:1935. [Crossref] [PubMed]
- Lahr MM, Luijckx GJ, Vroomen PC, et al. Proportion of patients treated with thrombolysis in a centralized versus a decentralized acute stroke care setting. Stroke 2012;43:1336-40. [Crossref] [PubMed]
- Rajan SS, Rajan S, Baraniuk S, et al. Implementing a Mobile stroke unit program in the United States: why, how, and how much? JAMA Neurol 2015;72:229-34. [Crossref] [PubMed]
- Walter S, Kostpopoulos P, Haass A, et al. Bringing the hospital to the patient: first treatment of stroke patients at the emergency site. PLoS One 2010;5:e13758. [Crossref] [PubMed]
- Weber JE, Ebinger M, Rozanski M, et al. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology 2013;80:163-8. [Crossref] [PubMed]
- Saifee TA, Burd CM, Koppel C. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology 2013;81:938. [Crossref] [PubMed]
- Lassalle L, Turc G, Tisserand M, et al. ASPECTS (Alberta stroke program early CT score) assessment of the Perfusion-Diffusion mismatch. Stroke 2016;47:2553-8. [Crossref] [PubMed]
- Grunwald IQ, Ragoschke-Schumm A, Kettner M, et al. First automated stroke imaging evaluation via electronic Alberta stroke program early CT score in a Mobile stroke unit. Cerebrovasc Dis 2016;42:332-8. [Crossref] [PubMed]
- John S, Stock S, Masaryk T, et al. Performance of CT angiography on a Mobile stroke treatment unit: implications for triage. J Neuroimaging 2016;26:391-4. [Crossref] [PubMed]
- Khatri P, Kleindorfer DO, Yeatts SD, et al. Strokes with minor symptoms: an exploratory analysis of the National Institute of Neurological Disorders and Stroke recombinant tissue plasminogen activator trials. Stroke 2010;41:2581-6. [Crossref] [PubMed]
- Dietrich M, Walter S, Ragoschke-Schumm A, et al. Is prehospital treatment of acute stroke too expensive? An economic evaluation based on the first trial. Cerebrovasc Dis 2014;38:457-63. [Crossref] [PubMed]
- Gyrd-Hansen D, Olsen KR, Bollweg K, et al. Cost-effectiveness estimate of prehospital thrombolysis: results of the PHANTOM-S study. Neurology 2015;84:1090-7. [Crossref] [PubMed]
Cite this article as: Liu R, Li W, Wang H, Qiu Z, Zi W, Zhang H. For “time is the brain”, what can be done prehospital. AME Med J 2017;2:81.

