Biopsy: bronchoscopy is best-interventional pulmonologists perspective
Introduction
Interventional pulmonology has bridged the gap between general pulmonology and thoracic surgery. Knowledge of pulmonary medicine along with extensive training in minimally invasive airway and lung procedures provides interventional pulmonologists with a unique perspective on the management of lung nodules. The ability to sample nodules using electromagnetic navigation bronchoscopy (ENB) along with biopsying mediastinal lymph nodes using endobronchial ultrasound (EBUS) bronchoscopy during one procedure brands bronchoscopy as the modality of choice for diagnosing and staging individuals with malignant lung nodules.
Lung cancer screening using low dose computer tomography (CT) has proven to be effective in decreasing mortality due to lung cancer in high-risk patients compared to radiographic screening (1). Although the majority of nodules identified on lung cancer screening CTs are benign, the high pre-test probability of cancer in screened patients requires physicians to have a low threshold to sample such lesions. As a result, any lung nodules identified on low dose CT scan during lung cancer screening must be followed with regular closely or sampled through modalities including bronchoscopy, transthoracic needle aspiration (TTNA), or surgical resection. While the various modalities used to biopsy lung nodules boast specific benefits, each has inherent risks.
ENB
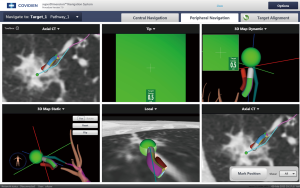
Tissue sampling of peripheral lung nodules is commonly performed bronchoscopically using ENB. This form of bronchoscopy is an image-guided localization procedure utilizing steerable catheters combined with highly specialized navigation software to create three-dimensional anatomical maps. The ENB system is comprised of an electromagnetic board, locatable guide, extended working channel, and a steerable catheter to sample lung nodules in intermediate and high-risk patients. By directing the locatable guide along the created pathway to peripheral lesions, in a manner similar to that of global positioning software (GPS), a bronchoscopist can perform brushings, biopsies, and washings of target nodules (Figure 1). Along with sampling peripheral lung lesions with ENB, physicians with advanced training in EBUS bronchoscopy are able to effectively biopsy lymph nodes in the mediastinum to determine a cancer stage during the same procedure. As a result, the ability to biopsy lung nodules and simultaneously stage the mediastinum makes bronchoscopy the ideal diagnostic modality to sample nodules identified through lung cancer screening.
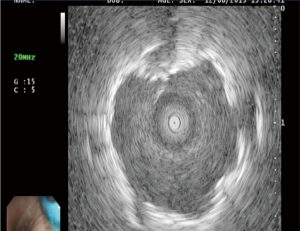
ENB is an effective and safe procedure. Peripheral lesions in the outer third of the chest less than 2 cm in diameter have a diagnostic yield of only 14% using conventional flexible bronchoscopy (2). Utilization of ENB in conjunction with use of a radial endobronchial ultrasound (R-EBUS) results in a yield of approximately 88% (Figure 2) (3). Additionally, the safety of the procedure is excellent, with a pneumothorax rate between 0–10% (4,5). Alternative options for sampling peripheral lung nodules include TTNA and surgical biopsy. Transthoracic needle aspiration is effective, with a yield of approximately 80%, the risk of pneumothorax associated with TTNA range anywhere from 5% to 64% (6-12).
EBUS bronchoscopy
While sampling peripheral lung nodules identified during lung cancer screening is essential, obtaining appropriate nodal staging may be equally as important in determining disease treatment. Patients are staged according to the tumor, node, metastasis (TNM) staging system based on tumor size, nodal station, and presence of metastases. The importance of nodal involvement is highlighted as 1- and 5-year survival significantly decreases in the presence of N1, N2, and N3 disease (13). Additionally, nodal staging has significant implications regarding potential curative surgery versus maintenance chemotherapy.
The American College of Chest Physicians (ACCP) recommendation for the mediastinal staging of patients with non-small cell lung cancer endorses EBUS bronchoscopy (14). Through real time ultrasound imaging, EBUS provides clear images of lymph nodes and proximal lung masses that can be adequately sampled through transbronchial needle aspiration (TBNA) (Figure 3). EBUS is a minimally invasive, outpatient procedure. Large studies investigating the use of EBUS for mediastinal staging have shown the procedure to be highly sensitive (93%) and specific (100%) while harboring an excellent safety profile (15). Pulmonologists with extensive training in performing EBUS bronchoscopy are capable of accurately staging the mediastinum by sampling lymph nodes as small as 5 mm. When peripheral lung nodules are sampled using ENB, the use of EBUS to stage the mediastinum is virtually always performed during the same procedure. As a result, unlike TTNA which does not offer access to mediastinal lymph nodes, advanced bronchoscopy utilizing EMN and EBUS to diagnose and stage lung cancer is the ideal to biopsy lung nodules identified through lung cancer screening.

CT and positron emission tomography (PET) for mediastinal staging
CT scans and PET scans have been used for clinical staging for patients with lung caner. Prior to the advent of EBUS bronchoscopy, mediastinoscopy was used obtain a mediastinal stage for patients with lung cancer and concern for N2 or N3 disease. While mediastinoscopy is highly sensitive and specific, it is invasive. Patients with lung nodules and the absence of lymph node enlargement or with a negative PET scans often go directly to surgery without histologic confirmation of N0 disease. Unfortunately, neither CT scanning nor PET scanning are optimal modalities for staging the mediastinum. Lymph node size is criterion used to distinguish benign from malignant lymph nodes and is inherently erroneous. The combined sensitivity of CT scanning for identifying malignant lymph nodes is 60–83%, with a specificity of 77–82%, and an accuracy of 75–80% (16,17). Although PET scanning harbors a higher sensitivity and specificity than CT in differentiating hyperplastic or reactive lymph nodes from metastatic lymph nodes, 79% and 91% respectively, it remains lower than that of EBUS bronchoscopy (17,18).
Conclusions
The escalating implementation of lung cancer screening represents a significant step for reducing lung cancer related mortality. In the process of detecting and treating lung cancer at early stages, screening implementation has identified a growing number of benign and malignant nodules. Because the majority of lung nodules identified through lung cancer screening are benign, it is essential that these nodules are biopsied through minimally invasive methods prior to resection. Additionally, if nodules are highly suspicious for malignancy, the mediastinum should be staged if lymphadenopathy is identified on a CT or PET scan. The ability of to safely and effectively biopsy nodules through ENB, along with simultaneous staging the mediastinum using EBUS, solidifies bronchoscopy as the most effective, safe, and expeditious means to guide treatment for lung nodules identified during lung cancer screening.
Acknowledgements
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ricardo Sales dos Santos, Myrna Godoy, Juliana Franceschini and Hiran C. Fernando) for the series “Update on Lung Cancer Screening and the Management of CT Screening Detected Pulmonary Nodules” published in AME Medical Journal. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.08.11). The series “Update on Lung Cancer Screening and the Management of CT Screening Detected Pulmonary Nodules” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Baaklini WA, Reinoso MA, Gorin AB, et al. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000;117:1049-54. [Crossref] [PubMed]
- Eberhardt R, Anantham D, Ernst A, et al. Multimodality bronchoscopic diagnosis of peripheral lung lesions: a randomized controlled trial. Am J Respir Crit Care Med 2007;176:36-41. [Crossref] [PubMed]
- Lamprecht B, Porsch P, Pirich C, et al. Electromagnetic navigation bronchoscopy in combination with PET-CT and rapid on-site cytopathologic examination for diagnosis of peripheral lung lesions. Lung 2009;187:55-9. [Crossref] [PubMed]
- Mahajan AK, Patel S, Hogarth DK, et al. Electromagnetic navigational bronchoscopy: an effective and safe approach to diagnose peripheral lung lesions unreachable by conventional bronchoscopy in high-risk patients. J Bronchology Interv Pulmonol 2011;18:133-7. [Crossref] [PubMed]
- Cox JE, Chiles C, McManus CM, et al. Transthoracic needle aspiration biopsy: variables that affect risk of pneumothorax. Radiology 1999;212:165-8. [Crossref] [PubMed]
- Li H, Boiselle PM, Shepard JO, et al. Diagnostic accuracy and safety of CT-guided percutaneous needle aspiration biopsy of the lung: comparison of small and large pulmonary nodules. AJR Am J Roentgenol 1996;167:105-9. [Crossref] [PubMed]
- Westcott JL. Percutaneous transthoracic needle biopsy. Radiology 1988;169:593-601. [Crossref] [PubMed]
- Khouri NF, Stitik FP, Erozan YS, et al. Transthoracic needle aspiration biopsy of benign and malignant lung lesions. AJR Am J Roentgenol 1985;144:281-8. [Crossref] [PubMed]
- Kazerooni EA, Lim FT, Mikhail A, et al. Risk of pneumothorax in CT-guided transthoracic needle aspiration biopsy of the lung. Radiology 1996;198:371-5. [Crossref] [PubMed]
- Laurent F, Michel P, Latrabe V, et al. Pneumothoraces and chest tube placement after CT-guided transthoracic lung biopsy using a coaxial technique: incidence and risk factors. AJR Am J Roentgenol 1999;172:1049-53. [Crossref] [PubMed]
- Klein JS, Salomon G, Stewart EA. Transthoracic needle biopsy with a coaxially placed 20-gauge automated cutting needle: results in 122 patients. Radiology 1996;198:715-20. [Crossref] [PubMed]
- Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest 2009;136:260-71. [Crossref] [PubMed]
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-e250S.
- Gomez M, Silvestri GA. Endobronchial ultrasound for the diagnosis and staging of lung cancer. Proc Am Thorac Soc 2009;6:180-6. [Crossref] [PubMed]
- Dales RE, Stark RM, Raman S. Computed tomography to stage lung cancer. Approaching a controversy using meta-analysis. Am Rev Respir Dis 1990;141:1096-101. [Crossref] [PubMed]
- Dwamena BA, Sonnad SS, Angobaldo JO, et al. Metastases from non-small cell lung cancer: mediastinal staging in the 1990s--meta-analytic comparison of PET and CT. Radiology 1999;213:530-6. [Crossref] [PubMed]
- Wu Y, Li P, Zhang H, et al. Diagnostic value of fluorine 18 fluorodeoxyglucose positron emission tomography/computed tomography for the detection of metastases in non-small-cell lung cancer patients. Int J Cancer 2013;132:E37-47. [Crossref] [PubMed]
Cite this article as: Mahajan AK. Biopsy: bronchoscopy is best-interventional pulmonologists perspective. AME Med J 2017;2:111.