
Thoracolumbar fractures classification using the smartphone
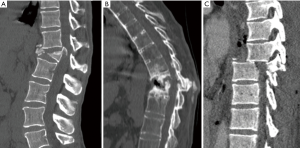
A recent clinical study found that diagnosing and classifying thoracolumbar fractures using a portable smartphone is as reliable as using a workstation-based picture archiving communication system (PACS) (1). This reliability is comparable to studies of reliability based on the use of PACS work-stations only (2). Substantial agreement for the AO and the Denis classifications was found. The AOspine thoracolumbar spine Injury classification system (AO-TLICS) strongly influences management, with fractures scoring more than five points considered surgical candidates (3); fractures classified as B2 fractures would score 6 points, B3 score 7 points, and C score 8 points (Figure 1). Unsurprisingly, a statistical correlation is seen between the agreement of fracture management and the grading of fracture severity using the AO-TLICS quantification score.
Intraobserver agreement was also demonstrated for the detection of neural canal penetration, however it is important to establish the existence of neurological injury as different areas of the spine can tolerate varying degrees of canal stenosis without any neurological compromise. For instance, there is a significant risk of neurological compromise when the canal narrowing is ≥35% at the level of the T11 to T12 vertebral bodies, ≥45% at L1 and ≥55% at the level of or below the L2 vertebral body (4). Neurological injury of the cord or cauda equina would score 4 points regardless of whether it is incomplete (N3 on the AO-TLICS classification) or complete (N4) and is an indication for emergency or urgent surgery. This shows the influence of canal stenosis in clinical management is based more on the clinical picture rather than image findings.
There was only a moderate intraobserver agreement for the quantification of loss of vertebral height and degree of kyphosis, though it should be noted that these parameters do not significantly influence management compared to accurate fracture classification. Interestingly, the AO-TLICS classification does not account for these two parameters, a fact regarded by some authors a flaw of the AO-TLICS classification (5). In patients with lower grade burst fractures, they would score 3 (A3) or 5 (A4) points, the decision to operate is based on the Surgeon’s preference, which may result in a delay to operate. In such cases, MRI may be indicated to rule out the frequently coexistent posterior ligament complex (PLC) injury. The PLC lesion is considered a case specific modifier in the AO- TLICS and its detection by MRI is consistent with a type B2 fracture and hence an indication for surgical treatment. On other hand, demonstration of PCL integrity, can change treatment to conservative therapy or to minimally invasive surgery, including vertebral augmentation (6). If the decision of conservative management has been taken in burst type A3 or A4 fractures, close follow-up is recommended due to the high likelihood of long-term kyphotic deformity or instability (5) (Figure 2). The two main factors which have been implicated in this progression are inadvertent injury of the PLC and intra-vertebral comminution and instability (7). Vertebral comminution and kyphotic correction are taken into account in the load-sharing classification system (8). Kyphotic correction is a sign of vertebral instability and can also be evaluated preoperatively by comparing the degree of kyphosis in extension CT scan with non-extension standing or sitting radiographs (9).
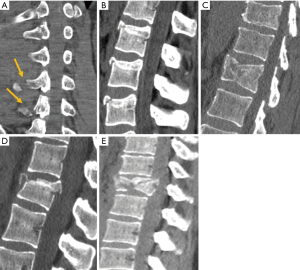
In summary, the article of Stahl et al. (1) reflects upon the current, mainstream practice of using messaging applications which have spread all over the world. Although Email consultations between doctors have been used for long time, instant messaging applications such as WhatsApp, have gained a foothold and are currently being used for quick consultations with colleagues who have no access to the PACS System. This practice will probably continue for long time in an unofficial way, although this could become a validated method in the discussion and management of vertebral fractures. The most emergent indications for spinal surgery are vertebral dislocation (C type) and neurological damage (N3, N4). Emergency doctors must be trained to identify neurological injury and the on call Radiologist must be also trained to accurate classify vertebral fractures, mainly when AO-TLICS is freely available on internet (10). Nevertheless, some institutions in the future might be interested in reducing cost by using cheaper smartphone-based teleradiology systems as a triage tool that may avoid the unnecessary transfer of non-surgical patients between hospitals, such as those with apophyseal (A0), Compression (A1) and split (A2) vertebral fractures but allows those patients with more severe injuries to be selected out and appropriately transferred to a tertiary spinal unit (Figure 2). In all these cases, clinical decision making has to rely on an accurate and thorough physical exam in addition to a powerful, polyvalent PACS system which has multiplanar reformat capabilities as well as the ability to generate 3D images.
Acknowledgements
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Ai-Min Wu (Department of Spine Surgery, Zhejiang Spine Surgery Centre, Orthopaedic Hospital, The Second Hospital and Yuying Children’s Hospital of Wenzhou Medical University, The Key Orthopaedic Laboratory in Zhejiang Province, Wenzhou, China).
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.10.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Stahl I, Dreyfuss D, Ofir D, et al. Reliability of smartphone-based teleradiology for evaluating thoracolumbar spine fractures. Spine J 2017;17:161-7. [Crossref] [PubMed]
- Urrutia J, Zamora T, Yurac R, et al. An independent interobserver reliability and intraobserver reproducibility evaluation of the new AOSpine Thoracolumbar Spine Injury Classification System. Spine (Phila Pa 1976) 2015;40:E54-8. [Crossref] [PubMed]
- Vaccaro AR, Schroeder GD, Kepler CK, et al. The surgical algorithm for the AOSpine thoracolumbar spine injury classification system. Eur Spine J 2016;25:1087-94. [Crossref] [PubMed]
- Hashimoto T, Kaneda K, Abumi K. Relationship between traumatic spinal canal stenosis and neurologic deficits in thoracolumbar burst fractures. Spine (Phila Pa 1976) 1988;13:1268-72. [Crossref] [PubMed]
- Mattei TA, Hanovnikian J, H, Dinh D. Progressive kyphotic deformity in comminuted burst fractures treated non-operatively: the Achilles tendon of the Thoracolumbar Injury Classification and Severity Score (TLICS). Eur Spine J 2014;23:2255-62. [Crossref] [PubMed]
- Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: An overview. Indian J Orthop 2015;49:72-82. [Crossref] [PubMed]
- Ruiz Santiago F, Tomás Muñoz P, Moya Sánchez E, et al. Classifying thoracolumbar fractures: role of quantitative imaging. Quant Imaging Med Surg 2016;6:772-84. [Crossref] [PubMed]
- McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994;19:1741-4. [Crossref] [PubMed]
- Nakamae T, Fujimoto Y, Yamada K, et al. Efficacy of Percutaneous Vertebroplasty in the Treatment of Osteoporotic Vertebral Compression Fractures with Intravertebral Cleft. Open Orthop J 2015;9:107-13. [Crossref] [PubMed]
- Available online: https://www2.aofoundation.org/wps/portal/surgery
Cite this article as: Ruiz Santiago F, Pérez Abela AL, Patel P. Thoracolumbar fractures classification using the smartphone. AME Med J 2017;2:164.

