Ruijin robotic thoracic surgery: right S6 segmentectomy
Clinical data
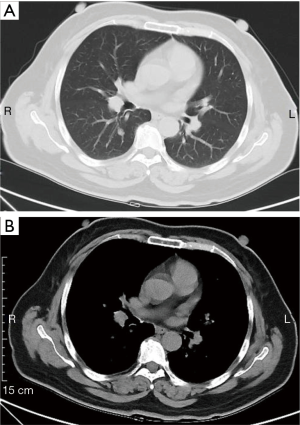
The patient was a 55-year-old woman admitted because of pulmonary nodules for 7 months detected by computed tomography (CT). A CT scan revealed a nodule in the right segment 6 (S6), which had enlarged during 7-month follow up. The patient’s syndrome did not include cough, shortness of breath, fever, or hoarseness. Her cardiopulmonary function, blood gas analysis, and laboratory tests were normal. There was no positive sign or supraclavicular lymph node enlargement on physical examination. She had no medical history. Survival of the patients who undergo segmentectomy is non-significantly worse (1,2) if the tumor size is smaller than 2.0 cm (3), but there is a functional advantage after radical segmentectomy compare with after a lobectomy (4). Therefore, we performed robotic-assisted right S6 segmentectomy for this patient with clinic stage IA lung cancer (Figure 1).
Operation steps
Anesthesia and body position
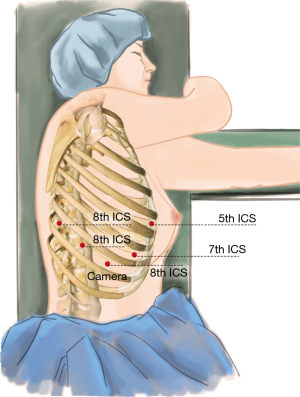
The patient received general anesthesia by double-lumen endotracheal intubation with single-lung (left) ventilation, and was placed in the lateral decubitus position and in a Jackknife position (Figure 2).
Ports
A 1.5-cm camera port (for a 12-mm trocar) was placed in the 8th intercostal space (ICS) at the right middle axillary line, and three separate 1.0-cm working ports (for 8-mm trocars) were made in the 5th ICS (#1 arm) at the right anterior axillary line, the 8th ICS (#2 arm) at the right posterior axillary line, and the right 8th ICS (#3 arm), 2 cm from the spine. An auxiliary port (for a 12-mm trocar) was made in the 7th ICS near the costal arch (Figure 3).
Installation of the surgical arms
The robot patient cart is positioned directly above the operating table and then connected. The #2 arm is connected to the bipolar cautery grab, and the #1 arm is connected to a unipolar cautery hook. An incision protector was used in the auxiliary port.
Surgical procedure
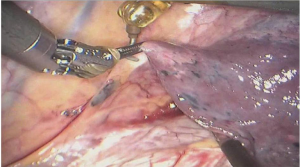
- The right inferior pulmonary ligament was exposed (Figure 4).
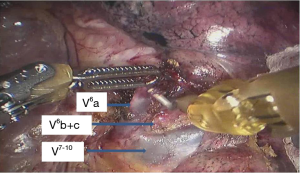
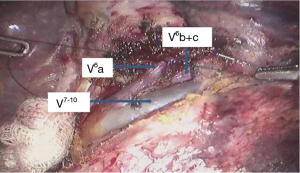
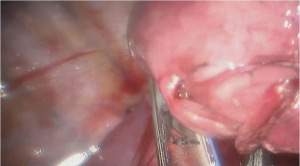
- Pulmonary veins V6a and V6b+c were identified (Figure 5).
- Vein V6a and preserve V6b+c (5) were cut (Figure 6).
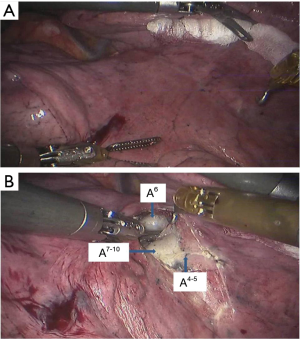
The interlobar fissure was exposed to facilitate a later pulmonary artery skeletonization (Figure 7).
- Artery A6 was cut (Figure 8).
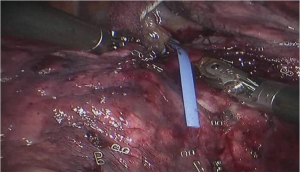
- Bronchus B6 was cut (Figure 9).
- The right lung was inflated and then deflated to show the inflation-deflation line. The S6 segmentectomy was completed along the simple intersegmental plane (Figure 10).
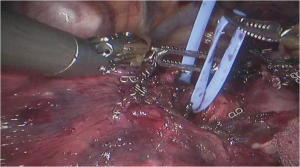
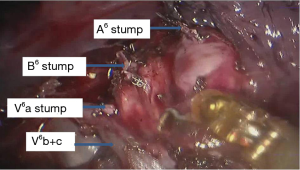
- The stumps were exposed (Figure 11).
Postoperative condition
The postoperative treatments include anti-inflammatory, and phlegm-resolving treatment. The drainage tube was withdrawn 2 days after surgery, and the patient was discharged 3 days after surgery. No complications were observed during hospitalization. Pathologic diagnosis was microinvasive carcinoma (pT1aN0M0), and all the lymph nodes were negative.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2017.01.11). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Keenan RJ, Landreneau RJ, Maley RH Jr, et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg 2004;78:228-33; discussion 228-33. [Crossref] [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Okada M, Nishio W, Sakamoto T, et al. Effect of tumor size on prognosis in patients with non-small cell lung cancer: the role of segmentectomy as a type of lesser resection. J Thorac Cardiovasc Surg 2005;129:87-93. [Crossref] [PubMed]
- Harada H, Okada M, Sakamoto T, et al. Functional advantage after radical segmentectomy versus lobectomy for lung cancer. Ann Thorac Surg 2005;80:2041-5. [Crossref] [PubMed]
- Nomori H, Okada M. Illustrated textbook of anatomical pulmonary segmentectomy. New York: Springer-Verlag, 2012.
Cite this article as: Li C, Yang S, Guo W, Jin R, Zhang Y, Chen X, Wu H, Du H, Han D, Chen K, Xiang J, Li H. Ruijin robotic thoracic surgery: right S6 segmentectomy. AME Med J 2017;2:23.