
Determining the management of sciatica
Sciatica is a common disease of middle age, but the management strategy has not yet been standardized. This is the reason for the article written by Ramaswami et al. (1). However, the determination of the management strategy seems to be too hasty from the information presented in this article.
First, the relevant dermatome of the lower lumbar nerve roots has to be identified, and the pain region confirmed in the left leg. If the pain is originating from the left L4/5 lumbar disc herniation (LDH), the left L5 nerve root is compressed. Thereby, the pain generally occurs mainly in the lateral part of the thigh and lower leg and/or medial part of the dorsum of the foot. However, Mr. Winston only complained of severe sharp and dull pain that originated in his left buttock and radiated to the dorsolateral aspect of his left thigh. His pain region did not completely coincide with a typical L5 dermatome. We sometimes experience the discrepancy of disturbed nerve root and the pain region. We therefore have to confirm that the pain originates from the compression of the corresponding nerve root. A nerve root block is the only examination that can clarify the discrepancy. If a similar radiating pain is observed during L5 nerve puncture or the pain resolves after lidocaine injection, it is strongly suggested that the pain originates from the left L4/5 LDH. In the absence of these two observations, other diseases such as superior cluneal nerve entrapment neuropathy, gluteus medius muscle pain, piriformis syndrome, and sacroiliac joint pain also merit consideration. Due to lack of space to explain each disease, we only discuss the possibility of misdiagnosis. To know the details of each disease, the readers can read the reference (2).
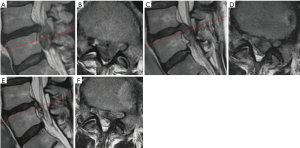
Second, even though the pain originates from the L4/5 LDH, the magnetic resonance imaging (MRI) findings need to be interpreted with caution. Presence of “left L4/5 LDH” did not explain the clinical manifestation. For example, the size of the herniated disc is a predictive factor of operative outcome. Carragee et al. reported that a longer anteroposterior disc length as well as larger ratios of disc to canal area were significant independent predictors of a good operative outcome (P<0.0001 both) (3). Not only the size but also the type of LDH is important for natural regression. Komori et al. reported that disappearance of herniated nucleus pulposus was seen frequently in cases of migrating LDH (4). Therefore, at least the size and type of LDH have to be determined before determining the management strategy. In case of small and/or migrating LDH, initially a combination treatment of physical therapy and medication (except for pregabalin) may be selected, as mentioned by Dr. Weinstein. Although highly migrating LDH has a tendency to resolve spontaneously, the process takes several months (Figure 1) (5). For early resolution of pain, enabling the patient to return to his job, surgery should be considered.
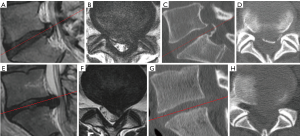
Mr. Winston is a 50-year-old bus driver. We also need to consider the presence of coincident spinal canal stenosis or calcified LDH (also known as “hard disc”). For the former case, the management strategy for lateral recess stenosis needs to be followed (this is also a controversial issue, and we will not discuss it here). In the latter case, spontaneous regression of calcified LDH cannot be expected, but the operative difficulty is greater than that in the case of non-calcified LDH. Because the calcified lesion often adheres to the nerve root and dura mater, the neural tissues are easily injured by rough operative procedures. We therefore have to perform computed tomography (CT) especially for elderly patients and/or in cases where a considerable time has elapsed since the diagnosis, so as to avoid the overlooking of the calcified lesion (Figure 2).
Assuming that the patient’s left L4/5 LDH is relatively large, non-migrating, and non-calcified, lumbar disc surgeries are promising for quick return to his job. However, we still have to discuss which kind of operation is better for this patient. Mr. Winston is highly overweight [body mass index (BMI) =35 kg/m2) and has mild chronic obstructive pulmonary disease (COPD, smoking one pack of cigarettes every day for 22 years). Thickened skin layers of obese patients occasionally disturb a conventional operative procedure such as open and microscopic discectomy, thereby prolonging the operation time. Prolonging the operation may increase the risk during the perioperative and postoperative periods. Moreover, the risks associated with general anesthesia, such as extubation failure, are greater for COPD patients than for those with normal respiratory function. Therefore, if a lumbar discectomy under local anesthesia is performed in a short time, the risks due to obesity and COPD can be avoided. Percutaneous endoscopic lumbar discectomy (PELD) is a minimally invasive operative procedure that meets these requirements. PELD is performed under endoscopic visualization, and the outer diameter of the endoscope is approximately 7 mm (6). We already have reported the superiority of PELD in obese patients (7). Furthermore, PELD can be performed under local anesthesia (6). In conclusion, if Mr. Winston’s condition meets the above-mentioned requirements, PELD should be selected as the surgical treatment.
Although a large number of clinical trials such as the Spine Patient Outcomes Research Trial (SPORT) and meta-analyses provide insight into the management of certain diseases, it is also important to consider the best personalized medical care for each patient based on the differences in conditions, predispositions, and social backgrounds.
Acknowledgements
We thank all the staff of our hospitals.
Funding: This work was partly supported by a grant from the Iwai Medical Foundation.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Ai-Min Wu (Department of Spine Surgery, Orthopaedic Hospital, Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Zhejiang Spine Surgery Centre, The Key Orthopaedic Lab of Zhejiang, Wenzhou, China).
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/amj.2018.02.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ramaswami R, Ghogawala Z, Weinstein JN. Management of sciatica. N Engl J Med 2017;376:1175-7. [Crossref] [PubMed]
- Kim K, Isu T, Morimoto D, Iwamoto N, et al. Common diseases mimicking lumbar disc herniation and their treatment. Mini-invasive Surg 2017;1:43-51. [Crossref]
- Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine (Phila Pa 1976) 1997;22:1650-60. [Crossref] [PubMed]
- Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976) 1996;21:225-9. [Crossref] [PubMed]
- Altun I, Yüksel KZ. Lumbar herniated disc: spontaneous regression. Korean J Pain 2017;30:44-50. [Crossref] [PubMed]
- Yeung AT. The Evolution and Advancement of Endoscopic Foraminal Surgery: One Surgeon’s Experience Incorporating Adjunctive Techologies. SAS J 2007;1:108-17. [Crossref] [PubMed]
- Koga H, Inanami H. Minimal laminectomy using the interlaminar approach for percutaneous endoscopic lumbar discectomy. Mini-invasive Surg 2017;1:56-62. [Crossref]
Cite this article as: Iwai H, Inanami H, Koga H. Determining the management of sciatica. AME Med J 2018;3:26.

