Etiology of priapism in the community: local factors can help guide prevention and savings
Introduction
Priapism describes a pathologically persistent condition arising from dysfunctional mechanisms regulating penile tumescence and flaccidity. It is defined as a full or partial erection lasting four hours or longer, beyond or unrelated to sexual stimulation (1). The incidence of priapism in the United States has been estimated to be between 5 and 8 emergency room visits per 100,000 (2,3).
Current understanding of the etiology and epidemiology of priapism includes certain medications and hematologic dyscrasias. However, our institution—located in Miami Beach, Florida—serves a patient population where we have noted that the more common etiologies for our priapism cases differ from what is commonly reported.
While multiple studies suggest that priapism is rarely medication induced, we find that these etiologies may vary significantly regionally, and may be evolving over time, especially with increased access to erectile medications through the internet and in “shot clinics”, where medications are provided with little oversight. Knowledge of the most prevalent etiologies in one’s home institution aids in prompt diagnosis of the cause, treatment, and most of all, prevention. Cognizance of the etiologies specific to one’s practice setting can help clinicians prevent a potentially devastating medical condition by improving patient education.
Methods
Data for this study were drawn from a tertiary care medical center and teaching hospital. Patient records at our institution were retrospectively reviewed after Institutional Review Board (IRB) approval (approval document number: 16-48-H-08). Emergent cases of priapism presenting to the emergency department and consulting Urologists were identified. These cases were screened for complete information with respect to past medical history (PMH), social history, and proximal cause of priapism, as well as treatment undergone and eventual outcome. Records were then reviewed further to better delineate medical history and identify those patients who had previously presented several times with priapism. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual consent for this retrospective analysis was waived.
Statistical analysis included chi-squared and Fisher exact tests to compare categorical variables (presented in the text as both quantities and percentages) and t-tests as well as ANOVA to compare continuous variables across two or more groups (continuous variable results are presented in the text as numbers and range). These were performed using IBM SPSS version 24.
Results
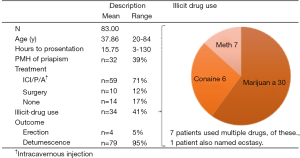
Between January 2014 and January 2015, 83 episodes of Priapism were recorded in 57 incident patients. Figure 1 summarizes these episodes, including those of non-incident patients. The majority of men were middle-aged and presented to the hospital after an average of 16 hours—all presenting with ischemic priapism. Most were treated effectively with intracavernosal injections (ICIs) of vasoconstrictive agents. Four patients refused treatment and accounted for all of the treatment failures. Fourteen episodes of priapism resolved spontaneously and over 70% of the remaining 69 episodes were successfully treated with ICI at bedside. In all, 10 episodes of priapism progressed to management under anesthesia. These included seven who underwent a shunting procedure - five performed as described by Winter’s technique, one as described by Al-Ghorab, and one by Quackel. Three other episodes of priapism required general anesthesia for effective irrigation and aspiration. Both those patients who were treated at bedside and those who proceeded to operative management achieved detumescence.
Additionally, there were four patients who refused treatment and left the hospital erect. Of these, one followed up in clinic, where he noted resolution of priapism and ability to achieve further erections with the use of Trimix. Over all, follow-up was limited to 9 incident cases (16%), all of whom described Trimix injection as a proximal cause of priapism (8 prescribed, including one in combination with a PDE-5-inhibitor, and 1 recreationally used). Of these, one refused treatment, one resolved spontaneously in the ED, one required a Winter’s shunt, one resolved with intracavernosal phenylephrine, and 5 resolved with a combination of phenylephrine and aspiration; all were able to achieve subsequent erections with the aid of prescribed Trimix.
Recreational drug use was common in the studied population. Most commonly, patients acknowledged using marijuana, but seven patients were admitted to using multiple drugs. Importantly, 10 of 34 drug-using patients admitted to using vasoactive substances—cocaine, crystal meth, and MDMA—though none of their priapisms were attributed to this drug use.
The most common comorbidity in our population was a history of HIV, seen in almost 40% of patients (Table 1). A history of metabolic disturbances—diabetes, hypertension (HTN), coronary artery disease (CAD), or dyslipidemia—was next most prevalent. Although these diagnoses co-occurred in multiple patients, at least one such diagnosis was seen in 13/57 unique patients (23%). Of note, only 5% of incident priapism episodes (3 unique patients) carried a history of hematologic dyscrasia, specifically sickle cell disease (SCD). These patients were each respectively seen for 1, 4, and 19 total episodes of priapism. SCD was assumed to be the primary cause of priapism in each of their presentations. Idiopathic priapism was suspected in 6 episodes in 6 unique patients.
Table 1
| Variable | Description | |
|---|---|---|
| N | % | |
| Hematologic dyscrasia | 3 | 5% |
| HIV | 20 | 31% |
| Diabetes | 5 | 8% |
| Psychiatric | 4 | 6% |
| Cardiac (HTN or CAD) | 9 | 14% |
| Dyslipidemia | 6 | 9% |
| Low testosterone | 1 | 2% |
| Prostate cancer | 3 | 5% |
| Other | 1 | 2% |
| Patient denied PMH | 2 | 3% |
| Missing information | 13 | 20% |
HTN, hypertension; CAD, coronary artery disease; PMH, past medical history.
The majority of incident cases (47 out of 57 episodes, or 82%) were presumed (by history taking) to be related to drug use; of these, a majority appeared to be due to recreational misuse of erectile dysfunction (ED) treatments (32 episodes or 56% of incident cases). This was defined as the use of medications without a prescription and without the supervision of a medical practitioner. The other 15 episodes (26% of incident cases) were evaluated in the context of adverse reactions to properly used prescription medications, which included trazodone [1], trimix [13], or phosphodiesterase-5 inhibitors (PDE5 inhibitors) [1]. Patients reported a history of illicit drug-use as well, but in none of the studied cases was this determined to be a causative factor for their priapisms. No cases of high-flow priapism episodes were recorded in the studied population. Amongst those patients who presented more than once with priapism (a total of 26 visits), 21 visits, or 81%, were related to SCD—the other 5 repeat visits were due to five unique patients each presenting twice. One of these five presented both times for priapism due to prescribed Trimix, and the other four experienced priapism following recreational use thereof, including one who combined it with a PDE-5 inhibitor.
ANOVA did not detect a significant difference between: prescription drug use, recreational drug use, hematologic dyscrasia, or idiopathic cause when comparing time to presentation (P=0.35). Compared with patients presenting with other etiologies, patients recreationally using ED treatments such as trimix differed in time to presentation significantly (P<0.01). We also reviewed the differences in time to presentation for other possible risk factors (Table 2). Notably, patients with a history of HIV or other sexually transmitted diseases (STIs) (one patient noted a history of HSV) appeared to present to the ED later when experiencing priapism (P=0.028). We had hypothesized that such patients, who are likely to be in more frequent contact with medical professionals for treatment of a sexually-transmitted disease may have a heightened awareness of priapism, but our data did not support this.
Table 2
| Tested risk factor | Mean time to presentation (hours) | P value* | ||
|---|---|---|---|---|
| With factor | Without factor | N | ||
| Prior ED | 17.5 | 15.1 | 83 | 0.687 |
| Multiple episodes | 14.6 | 16.7 | 83 | 0.634 |
| Recreational drug use | 17.2 | 13.6 | 83 | 0.354 |
| PMH of HIV or STI | 26.0 | 12.4 | 59 | 0.028 |
| Recreational use of ED treatment | 22.7 | 10.4 | 83 | <0.01 |
*, populations compared using independent sample t-test. ED, erectile dysfunction; PMH, past medical history; STI, sexually transmitted disease.
Neither multiple previous episodes of priapism nor a history of illicit drug-use were associated with a difference in time to hospital (P=0.634 and 0.354, respectively). Similarly, prior documented history of ED (P=0.687), also thought to correlate with a heightened awareness of sexual dysfunction and priapism, did not predict any difference in time to presentation. The only noted possible predictors of delayed presentation—recreational use of ED treatments and STI history—were combined in a multivariate linear regression model, which showed significant overlap in these populations (23 of 24 patients with STI history had misused ED medication) and that only patients who had no history of either predictor appeared more likely to present sooner (P<0.01).
Because patients misusing ED medications represented a disproportionate burden of priapism episodes, we further explored this subset. Of the 32 incident presentations attributed to misused ED medicines, 27 provided past medical history. Eight were HIV negative, and 19 were HIV positive (70.4%), a distribution which contrasted with the overall population and the population of priapism due to other causes (P<0.01, Pearson Chi Squared Test).
Moreover, the patients who presented following misuse of ED treatments were also nominally more likely to use other drugs recreationally. Of these 32 cases, 10 (31%) occurred in patients also using illicit drugs, compared to only 3 (12%) among priapisms of different etiology (P=0.117, Fisher Exact Test).
Discussion
Since the 1980s, medical literature has described numerous etiologies of priapism, identifying idiopathic causes as most common. Patients presenting with priapism for different reasons compelled us to undertake a retrospective review to better categorize the etiology of priapism at our institution. Our series suggests that national data about priapism should be contextualized locally to improve patient education and prevention, especially considering this condition’s significant economic impact.
A 1986 study of 230 cases reported 56% of priapism cases to be idiopathic, while 21% were associated with alcohol or drug use or abuse, 12% were associated with perineal trauma, and 11% were associated with hematological dyscrasias, such as SCD (4). Another study conducted in 2012 of 115 patients reported 69% of cases to be unrelated to ED medication treatment, 12% idiopathic, 9% associated with drug use or abuse, 8% related to prescription drug use, and 3% associated with hematologic dyscrasias (5). Another 2013 review concurred that most cases of priapism are idiopathic (6).
In strong contrast to evidence in the current literature, the prevalence of hematologic dyscrasia, such as SCD, appeared to account for only 5% of our incident cases. An overwhelming 82% of incident priapism was associated with some form of drug use (both recreational and prescribed substances, including illicit drugs) rather than hematologic dyscrasia or trauma. Drug use was still the cause in 63% of total cases (incident and non-incident), even when counting the handful of patients who re-presented many times due to sickle cell. This finding is especially worrisome given the rise in “shot clinics”, which provide such medications with little oversight, as well as the increased access to these drugs online. These drugs then filter to individuals with little questionable for them, which we surmise may lead to our high rate of priapism.
Smith et al. found that this increased accessibility has facilitated the misuse of these medications and that the use in social settings has gained popularity, both in young, healthy patients, as well as those with chronic medical conditions, including HIV infection (7). A study by Capogrosso et al. states 22–78% of patients using PDE5 inhibitors obtain these medications without a medical prescription, which indicates a wide range of variability regarding use (8). Furthermore, Musacchio et al. studied fourteen participants aged 18–25 from universities in Chicago who reported using ED drugs such as a PDE5 inhibitors like Viagra. They found that 54% of these drugs were obtained from friends and 39% from other non-medical sources such as the internet (9). Similarly, Schnetzler et al. found that 32% of their study participants using PDE5 inhibitors obtained these medications without prior healthcare professional interaction. Based on these findings along with the risks associated with PDE5 inhibitor use from uncontrolled sources, they encourage providers to actively address ED and to discourage men from seeking ED medications from uncontrolled sources (10).
We moreover found that patients misusing ED drugs were also more likely to have had a history of sexually transmitted disease. Of note, recreational drug use, including marijuana, cocaine, and crystal meth, was prevalent. Of these cases, 70% were reported as HIV positive and 31% admitted to recreational drug use. The remaining cases were adverse reactions to prescribed medications—trazodone, trimix, and PDE5 inhibitors. In all, our population indicates that hematologic causes may not be common in all communities, and that providers should consider the misuse of ED treatment and sexual risk behaviors when attempting to better triage and prevent priapism in the community.
These results contrast with those classically reported in the literature (Figure 2). For all the studies that we reviewed, a total of 248 of 634 patients (39%) had an idiopathic etiology versus 6 of 57 patients (11%) at our own institution. For drug related priapism, there were 184 cases out of 634 individuals (29%) in the collective studies versus 47 out of 57 incident cases (82%) at our institution. For those studies that evaluated patients with hematologic dyscrasia etiology, 1,865 patients out of 9,165 individuals (20%) had this etiology versus 1 out of 19 (5%) at our institution. Two other etiologies were described in other studies but the data was not available for our institution. In the literature reviewed, traumatic etiology comprised 14 cases out of 115 (12%), whereas we saw no patients with this etiology. Before the last decade, studies identified more than half of all priapism cases as idiopathic in nature (4,11). Needless to say, much has changed since priapism etiology was first studied, including the dissemination of erectile medications.
In a 2013 review, Roughmann et al. reported that hematologic dyscrasias, such as SCD, were identified as the most common precipitating cause of priapism in a national sample (2). In other studies, SCD was determined as less prevalent (21%) than previously documented (3). In our incident cases, however, the contribution of SCD patients to the total ED cases remained a minority (5%).
In the same review, Roughmann also found that only 3.6% of all priapism cases in a nationwide sample of emergency departments were associated with a history of drug use (2). Similarly, Gottsch et al. also reported drug use as a minority cause of priapism; of 115 cases in their study, 17% were associated with drug use (8% drug—prescribed and 9% as other—drug user) (5). Furthermore, the use of oral medications and intracavernous injections, such as prostaglandin, papaverine, and phentolamine, has been a noted cause of priapism but has been consistently reported to account for a small proportion of etiologies (6). Unlike previous findings, the vast majority of our priapism patients presented because of drug use, most of which were used improperly or recreationally.
Perhaps even more unique to our series is the high prevalence of HIV—listed for almost 40% of our patients’ medical histories. No large studies have reported a correlation between HIV history and priapism, with Gottsch et al. noting a comorbid HIV diagnosis in only 3.5% of their sample. This likely represents the high local prevalence of HIV rather than any causal relationship, though it requires further evaluation.
In a study similar to our own, an audit of priapism cases in Perth, Australia over a 16 year period, 1985–2000, yielded 82 episodes of priapism recorded in 63 patients (12). The majority of episodes, 62 total incidents in 48 individual patients, were related to use of ICI therapy for ED (12). They suggested that their findings may be related to the years studied—noting the mentioned changes in ED treatments—as well as to their metropolitan environment.
In recent years, targeted community-interventions have worked successfully in reducing the HIV-AIDs epidemic around the world; thus, communities like ours may be uniquely positioned to utilize existing patient-engagement strategies to better prevent priapism in a likewise fashion. Drug use, whether recreational or prescribed, as a majority cause of priapism at our institution, coupled with the risk of STI, lends itself readily to improvement through behavior modification, which can have striking economic implications for any hospital.
Analysis of the Nationwide Emergency Department Sample (NEDS) and Healthcare Cost and Utilization Project (HCUP) estimated that this small proportion accounts for an average annual expenditure of more than $1 million dollars on priapism alone (3). Inpatient admissions from such emergency department visits cost an average of $41,909 each and are responsible for 86.8% of this total annual cost (3). Thus, prevention should be maximized. In fact, efficient management of patients through outpatient interventions may lower costs to less than $2,000 per case (3) in addition to improving patient outcomes by minimizing unnecessary and potentially dangerous hospitalizations. Because almost 60% of our yearly priapism consults are related to misuse of ICI and other ED medication, we believe that the chronicity of ED—which necessitates increased primary and specialty care visits—can be harnessed to induce behavior modification and reduce emergency presentations for priapism significantly. This is especially true when considering that our analysis indicates that these patients are either similar to or delayed compared to their peers in presenting with priapism for medical treatment. Utilizing their chronic sexual-medicine visits to educate about priapism and proper use of ED medications should, at the least, allow them to more quickly identify a problem and present for evaluation.
As such, our department has already started working with affiliated infectious disease and primary care physicians to convey the dangers of misusing ED medications as a means of mitigating emergency presentations.
Our study suffers from certain limitations in generalizability and sample size. Firstly, it is a limited retrospective study. Additionally, our patient population showed limited follow-up (16%), and although the purpose of our study was to clarify the etiologies of priapism, this limitation as well as the lack of objective IIEF criteria for judging erectile function before and after intervention make contextualization of the results challenging. Furthermore, not all communities resemble ours and our results should not be treated as an overhaul of the national causes of priapism. Of course, our results may be externally valid for institutions in similar major metropolitan areas that are subject to an increased incidence of misuse of ED treatment. For other urologists, our findings indicate a need to assess one’s own community and to better contextualize literature assumptions about the causes of priapism therein.
Conclusions drawn from larger databases may lack extenuating or explaining information that can only be gleaned from local medical records. Identifying cases from nationally reported data by ICD-9 code alone risks the unintentional inclusion of repeat presentations of patients with priapism and may leave researchers unable to decipher within the sample population (3). Thus, our results urge a re-examining of local factors influencing priapism presentations, which may reveal other methods for mitigating risk, depending on practice setting.
Conclusions
By identifying a community-specific etiology of priapism, we were able to establish the high-risk population at hand. This interpretation provides clarity in addressing emergency department cases and administering the most safe and effective care to resolve a non-life threatening, yet medically urgent complication. Most importantly, such analysis allows us to better prevent a costly and distressing condition for our patients.
Our analysis provides an updated understanding of etiologies from those previously available, highlighting the fact that different communities may experience entirely different etiologies for medical conditions at different time points. Thus, nationally derived statistics must be contextualized locally to improve prevention and to decrease the costly utilization of emergency services.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj.2020.01.04/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Patient records at our institution were retrospectively reviewed after Institutional Review Board (IRB) approval (approval document number: 16-48-H-08). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Broderick GA, Kadioglu A, Bivalacqua TJ, et al. Priapism: pathogenesis, epidemiology, and management. J Sex Med 2010;7:476-500. [Crossref] [PubMed]
- Roghmann F, Becker A, Sammon JD, et al. Incidence of priapism in emergency departments in the United States. J Urol 2013;190:1275-80. [Crossref] [PubMed]
- Stein DM, Flum AS, Cashy J, et al. Nationwide emergency department visits for priapism in the United States. J Sex Med 2013;10:2418-22. [Crossref] [PubMed]
- Pohl J, Pott B, Kleinhans G. Priapism: A three-phase concept of management according to etiology and prognosis. Br J Urol 1986;58:113. [Crossref] [PubMed]
- Gottsch HP, Berger RE, Yang CC. Priapism: comorbid factors and treatment outcomes in a contemporary series. Adv Urol 2012;2012:672624. [Crossref] [PubMed]
- Burnett AL, Sharlip ID. Standard operating procedures for priapism. J Sex Med 2013;10:180-94. [Crossref] [PubMed]
- Smith KM, Romanelli F. Recreational use and misuse of phosphodiesterase 5 inhibitors. J Am Pharm Assoc (2003) 2005;45:63-72; quiz 73-5. [PubMed]
- Capogrosso P, Ventimiglia E, Oreggia D, et al. Medical treatment of erectile dysfunction: Too many medical prescriptions? Urologia 2017;84:121-9. [Crossref] [PubMed]
- Musacchio NS, Hartrich M, Garofalo R. Erectile dysfunction and viagra use: What's up with college-age males? J Adolesc Health 2006;39:452-4. [Crossref] [PubMed]
- Schnetzler G, Banks I, Kirby M, et al. Characteristics, behaviors, and attitudes of men bypassing the healthcare system when obtaining phosphodiesterase type 5 inhibitors. J Sex Med 2010;7:1237-46. [Crossref] [PubMed]
- Kulmala RV, Lehtonen TA, Tammela TL. Priapism, its incidence and seasonal distribution in Finland. Scand J Urol Nephrol 1995;29:93-6. [Crossref] [PubMed]
- Earle CM, Stuckey BG, Ching HL, et al. The incidence and management of priapism in Western Australia: a 16 year audit. Int J Impot Res 2003;15:272-6. [Crossref] [PubMed]
Cite this article as: Wayne G, Weisberg M, Monreal A, Atri E, Wong V, Nieder AM, Caso J, Polackwich AS. Etiology of priapism in the community: local factors can help guide prevention and savings. AME Med J 2020;5:26.