
A case of pleural thymoma presenting as bilateral pleural based mass
Introduction
Thymoma is a tumour of epithelial origin, which arise from epithelium of thymus gland (1). It’s a rare neoplasm with incidence of 0.15% cases per 100,000 person/year (2). It is the most common primary neoplasm of anterior mediastinum and it commonly affects patient aged between 40–60 years with equal gender predilection. Ectopic thymoma is rare where it accounts for only 4% of all thymoma (3). Ectopic thymoma can be found in the neck, trachea, lung, thyroid and rarely pleura. Interesting to note, most of the reported cases of pleural thymoma usually involve one side of thorax. Here, we report a case of pleural thymoma presenting as bilateral pleural based mass. To our best knowledge, this is the first reported bilateral pleural thymoma in our region. In addition, there was absent of mediastinal thymoma in this patient.
Case presentation
A 73-year-old lady with no known medical illness presented a month ago with gradual onset worsening difficulty in breathing for 2 months duration. It was associated with dry cough, loss of appetite and loss of weight of 5 kg. She denied fever, chest pain or heart failure symptoms. She has no smoking history or relevant occupation history. On examination, she was comfortable and not tachypneic but appeared cachexic. Her vital signs were normal. Respiratory examination showed reduced air entry bilaterally and dullness on percussion of lower zone. Cardiovascular, abdominal and neurological examinations were normal. There was no palpable lymph node. There were no signs of myasthenia gravis as well. All procedures performed in this study were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
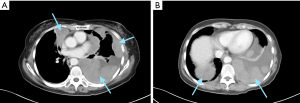
Her full blood count, renal function and liver function test were normal. Her electrocardiography and echocardiography were normal. Her chest radiograph showed bilateral lower zone opacity, hence proceeded with computed tomography (CT) of thorax. It showed bilateral nodular mildly enhancing pleural mass, with left measuring 6.2 cm × 9.9 cm × 17.1 cm and right measuring 5 cm × 3.1 cm × 8.6 cm (Figure 1). There was presence of left pleural effusion as well. Given the CT findings, the differentials diagnosis were metastasis, lymphoma, mesothelioma or benign tumour.
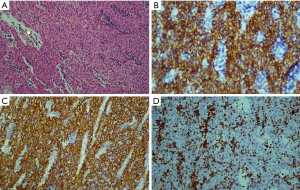
Subsequently, an ultrasound guided biopsy of right pleural mass was done. 2 weeks later, the biopsy report returned. The biopsy showed fragment of fibrous tissue infiltrated by sheet-like neoplastic epithelial cells admixed with non-neoplastic lymphocytes cells. Immunohistochemical study showed diffuse strong positivity to CK AE1/AE3, positivity to CK5/6, P63, CD5, CD4,5 and TdT (Figure 2). It confirmed the diagnosis of pleural thymoma, type B3 (80%) and B2 (20%), Masaoka stage 4. The tumour was negative for CD5 and CD117, excluding thymic carcinoma. Patient was then referred to oncology team. On assessment in oncology clinic, patient was comfortable but appeared cachexic. A multidisciplinary team meeting was held and it was deemed that patient was not suitable for surgical intervention. Patient was then started on chemotherapy regime with intravenous carboplatin at dose of area under curve 5 and intravenous paclitaxel at dose of 75 mg/m2. She tolerated the chemotherapy with no adverse event. She was planned for interval CT scan after 4 cycles of chemotherapy.
Discussion
Pleural thymoma is a rare entity, which has been rarely described in the literature. The pathogenesis of ectopic thymoma is likely to be related to the embryogenesis of thymus gland. Developmentally, the thymic epithelium originates in the third or fourth branchial pouches and descends caudally with the third parathyroid into the anterior mediastinum. Aberrant migration of thymic tissue can occur anywhere along this pathway which can result in ectopic thymic tissue. Ectopic thymoma is believed to originate from these ectopic thymic tissue (4).
Clinically, the presentation of thymoma is diverse. Most of them are rather asymptomatic and diagnosed incidentally from chest radiograph or CT thorax (2). On the other hand, patient with ectopic thymoma can present with chest pain, respiratory difficulty or constitutional symptoms like our patient. Some may present with symptoms of compression such as superior vena cava syndrome or dysphagia. Chest radiograph typically shows pleural thickening with encasement of the lung or pleural mass lesions. On CT thorax, it may appear as one or more pleural nodules. After iodinated contrast, thymoma are characterized by homogenous enhancement (2). The differential diagnosis to consider are solitary fibrous tumour of pleura, mesothelioma, metastatic tumour or sarcoma of the chest wall (5).
The diagnosis of thymoma requires biopsy and histopathological examination. In general, thymoma can be classified into A, B or C according to World Health Organisation (WHO) classification (2). On microscopic examination, the tumour typically shows a dense lymphoid process with lobular configuration separated by fibrous septa. It shows biphasic cells population with neoplastic epithelial cells and lymphoid cells. Immunohistochemical staining can further characterise the tumour. The epithelial cells typically show immunoreactivity to CKAE1/AE3, CK5/6 and p63 protein. The T lymphocytes in the tumour express immunoreactivity towards terminal deoxynucleotidyl transferase (TdT) and CD99. On the other hand, PAX-8, CD5 and CD117 are able to differentiate thymoma from thymic carcinoma (6).
The management of thymoma is mainly multidisciplinary approach. In general, it should involve the discussions between medical and radiation oncologists, pathologists, radiologists, thoracic surgeons and possible neurologists when patient has myasthenia gravis. Surgical resection remains the mainstay of treatment of resectable thymoma. Adjuvant chemoradiation should be considered based on staging and resection status (7). Besides that, chemotherapy and radiotherapy are also options for non-surgical candidates. Combination of different treatment modality frequently associated with better outcome.
Our case is an elderly lady presented with dry cough, difficulty in breathing and constitutional symptoms for 2 months. CT thorax showed bilateral nodular enhancing pleural based mass. Given the rarity of pleural thymoma, we did not consider pleural thymoma as our differential diagnosis. Our differential diagnosis were lymphoma and mesothelioma given that these are more common pathology. The strength of this case is accurate diagnosis by histopathological examination and immunohistochemistry. The complete staining enables us to clinch the diagnosis and hence, appropriate treatment can be given to the patient. However, our case is limited by lack of experience and literature on management of bilateral pleural thymoma. It remains as a single case in our centre.
Conclusions
Pleural thymoma is a rare entity. Clinicians need to consider this as a differential diagnosis in approaching pleural mass. Diagnosis is often obtained by histopathological examination. Immunohistochemical testing of tissue is pivotal in diagnosing thymoma, differentiating thymoma from lymphoma. Management of thymoma is by multidisciplinary discussion.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj.2019.11.05/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fukayama M, Maeda Y, Funata N, et al. Pulmonary and pleural thymoma. Diagnostic application of lymphocyte markers to the thymoma of unusual site. Am J Clin Pathol 1988;89:617-21. [Crossref] [PubMed]
- Picchi E, Di Giuliano F, Ferrari D, et al. Pleural thymoma: Radiological and histological findings. Eur J Radiol Open 2018;5:147-52. [Crossref] [PubMed]
- Filosso PL, Delsedime L, Cristofori RC, et al. Ectopic pleural thymoma mimicking a giant solitary fibrous tumour of the pleura. Interact Cardiovasc Thorac Surg 2012;15:930-2. [Crossref] [PubMed]
- Yamazaki K, Yoshino I, Oba T, et al. Ectopic pleural thymoma presenting as a giant mass in the thoracic cavity. Ann Thorac Surg 2007;83:315-7. [Crossref] [PubMed]
- Elkolaly RM. Pleural thymoma: our first case. Egypt J Bronchol 2016;10:79-81. [Crossref]
- Qing G, Ionescu DN, Colby TV, et al. A 75-year-old man with an asymptomatic pleural-based mass discovered on routine chest radiographs. Primary pleural thymoma. Arch Pathol Lab Med 2006;130:e62-5. [PubMed]
- Roden AC, Molina JR. Editorial: pleural recurrence of thymoma—what is the value of intra-thoracic chemo-hyperthermia? J Thorac Dis 2017;9:3583-6. [Crossref] [PubMed]
Cite this article as: Cheo SW, Choo NJ, Low QJ, Abu Bakar NA, Voon PJ. A case of pleural thymoma presenting as bilateral pleural based mass. AME Med J 2020;5:12.

