
Granulomatosis with polyangiitis presenting as renal mass: a literature review of imaging findings
Introduction
Granulomatosis with polyangiitis (GPA), formerly called Wegener’s Granulomatosis, is a chronic antineutrophil cytoplasm antibody (ANCA)-associated vasculitis having both granulomatosis and polyangiitis component. It causes vasculitis of small and medium sized vessels, mainly of upper and lower respiratory tract and kidneys (1). Renal involvement may be seen in 20% patients at initial presentation, and ultimately 80% patients with GPA may have renal involvement (2). Most common renal manifestation is segmental glomerulonephritis with proteinuria (3). Extremely rare is GPA renal manifestation as a renal mass. To knowledge, there are only 22 reported cases in literature on GPA manifesting as a renal mass, with the first case being described by Maguire et al. in 1978 (4). After a search of literature on GPA renal involvement in the form of renal masses, mainly the pathology and management has been described, with limited description of imaging findings. This review tries to compile all these cases, emphasizing on the imaging findings found in those cases, with a table summarizing those findings. We present the following article in accordance with the Narrative Review reporting checklist (available at https://amj.amegroups.com/article/view/10.21037/amj-21-50/rc).
Methods
Using PubMed Medline index and Google search, existing English language case reports were searched using key words (GPA, granulomatosis with polyangiitis, Wegener’s, pseudotumor, renal cell carcinoma, renal mass) on 12/30/2021 and references of relevant studies and case reports were also included. So far, there are only 27 reported cases in literature on GPA manifesting as a renal mass, a with the first case being described by Maguire et al. in 1978 (4). Clinical and imaging (US, CT scan and MR) data, when available were tabulated from all the existing case reports (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | 30/12/2021 |
| Databases and other sources searched | PubMed/Medline index and Google search |
| Search terms used | GPA, granulomatosis with polyangiitis, Wegener’s, pseudotumor, renal cell carcinoma, renal mass |
| Timeframe | 1978 to 2021 |
| Inclusion and exclusion criteria | Inclusion: all cases of GPA presenting as renal mass in English literature; exclusion: non-English literature |
| Selection process | Selection performed by both authors; first author conducted selection till 2018 and author 2 from 2018 onwards |
GPA, granulomatosis with polyangiitis.
Results
A total of 27 cases of GPA presenting as renal mass were found ranging in publication from 1978 to 2021. US was performed/described in 14/27 cases, CT scan in 23/27 and MRI in 5/27 cases. 4/27 cases reported more than one mass, while rest had only one mass. All the cases, including their major clinical and imaging features are summarized in Table 2. Additionally, Table 3 describes the summary of the most common characteristic imaging features of these lesions.
Table 2
| Case | Clinical | USG | CT | MRI | Other | Comment |
|---|---|---|---|---|---|---|
| Maguire 1978 (4) | None | None | None | None | Urography showed unilateral single upper pole mass distorting calyx; arteriography showed peripheral pruning s/o glomerulonephritis | First case of renal mass |
| Schapira 1986 (5) | 45-year-old male with nasal polypectomies, cavitating right lung mass with proteinuria; ANCA unknown | Thick posterior cortex compressing PCS | None | None | Urography showed large mass left lower pole which was avascular on angiography; gallium scan uptake in lung and kidney | Nephrectomy done f/b diagnosis f/b cyclophosphamide f//b improvement |
| Schydlowsky 1992 (6) | 47-year-old man with polyuria polydipsia with bitemporal hemianopsia; ANCA (+) C3d (+) | 5.5 cm × 5.1 cm tumor like mass left kidney | Increased density in perirenal fat and fascia thickening with hypoenhancing lesion left kidney s/o inflammatory lesion | None | Tc 99 scan showed slightly avid tumor like mass LK | Nephrectomy done |
| Smith 1993 (7) | 52-year-old Asian woman presented with a 2-month history of left loin pain, intermittent fever, night sweats, weight loss and episclerotic nodule; ANCA unknown | Left renal mass | Left renal mass | None | None | Nephrectomy |
| Fairbanks 2000 (8) | 68-year-old male with fever, weight loss and ear pain and normal urinalysis; pANCA (+) | None | Two hypoenhancing infiltrating mass lesion in posterior part LK which took shape of kidney, suspicion of lymphoma or TCC | None | CT of the chest showed an irregular 2-cm mass in the left lung apex, moderate right hilar lymphadenopathy, and a posterior segment infiltrate in the right lower lung | No nephrectomy done, diagnosis on biopsy f/b medical management |
| Verswijvel 2000 (9) | 24-year-old male with fatigue, fever, night sweat and hematuria; cANCA (+) | Left renal upper pole mass with slightly hyperechoic periphery and hypoechoic centre | Isodense hypoenhancing mass with central portion more hypoenhancing than periphery | T1 isointense and T2 hypointense (with central hyperintensity) hypoenhancing mass with minimal calyceal compression | Lesion confused with lymphoma on imaging; Pt also had left splenic infarct | Medical management, f/u USG 6 months later showed resolved renal mass |
| Carazo 2001 (10) | 29-year-old man with history of pain in the left flank, fever, and night sweats for 2 weeks; ANCA (+) | Multiple isoechoic masses without vascularization | B/L round mildly hypodense (23–25 HU) centrally hypo-non enhancing renal masses with cortical rim enhancement | None | Follow up CT showed RK disease resolution but LK disease worse with perirenal extension; arteriogram showed left renal vasculitis | Diagnosis made on biopsy, but left nephrectomy ultimately required |
| Kapoor 2002 (11) | 22-year-old male with fever, hematuria and raised creatinine; cANCA (+) | Large bilateral echogenic masses | None | B/L multiple round, parenchymal lobular increased signal intensity areas distorting calyses | None | Diagnosis on biopsy f/b dialysis |
| Sichani 2012 (12) | 22-year-old female with fever of unknown origin; had left mastoidectomy in past; ANCA (+) | 6 cm heterogenic mass in upper and lower pole | Hypodense mass at the left kidney suggesting a renal abscess, tumors or infiltrative lesions like lymphomas | None | None | Suspected renal abscess; Pt died post biopsy |
| Leung 2004 (13) | 66-year-old male with fever, weight loss, left flank pain; pANCA (+) | Multiple solid 2-3 cm renal masses | Hypoenhancing multiple masses | None | FNAC showed lymphoma; surgical exploration showed diagnosis | Medical management; F/U CT after 6 months showed resolved lesion |
| Krambeck 2005 (14) | 61-year-old male with weight loss, night sweat, cough, sinusitis; cANCA (−) |
None | 5.2-cm, solid, hypoenhancing mass in the lower pole RK | None | cANCA negative; Pt had chronic rhinosinusitis, parasellar meningioma and diagnosis of RCC suspected | Partial Nephrectomy, f/b diagnosis f/b medical management |
| Negi 2006 (15) | 40-year-old male with fever, flank pain and epistaxis; cANCA (+), anti-PR3 (+) | None | Hypoenhancing left renal upper pole mass s/o renal abscess or atypical RCC | None | on prebiopsy 6 weeks CT scan, mass spontaneously resolved and new small renal lesions seen | Medical management |
| Vandergheynst 2015 (16) | 32-year-old male with left lower quadrant pain, polyarthralgia, hypoesthesia of fingers and toes, proteinuria; cANCA/anti-PR3 (+) | None | Left kidney hypoenhancing lower pole mass with infiltration of perirenal fat | None | Imaging s/o of renal cancer, adenocarcinoma or lymphoma | Diagnosis made on biopsy |
| Roussou 2008 (3) | 72-year-old male with fever, ear pain and headache; pANCA (+) | None | 4 cm lower and 1.3 cm midpole two LK masses | Hypoenhancing left renal masses | None | Left nephrectomy for RCC suspicion |
| Boubenider 2008 (17) | 45-year-old female with fever, epistaxis, skin rash; cANCA was (+) at an outside facility but (−) after admission to authors’ institution | Small irregular atrophic LK with irregular mass like hyperechoic lesion RK upper pole | Mass like expansion upper pole RK; isodense lesion | None | Suspicion of tuberculosis made; Pt had renal failure | Nephrectomy done |
| Frigui 2009 (2) | 59-year-old female with fever, weight loss and ocular redness; cANCA/anti-PR3 (+) | B/L nephromegaly | B/L hypodense multiple non-enhancing upper pole masses; largest RK 6×3.5, LK 5.5×3 | none | Suspicion of lymphoma or inflammatory pseudotumor | Diagnosis made on biopsy f/b medical Mx; F/U CT 6 months, partial resolution, at 1-year full resolution |
| Dufour 2012 (18) | 70-year-old male with weakness, sinusitis, cough, dyspnea, and mononeuritis multiplex; pANCA/anti-MPO (+) | None | Solid, enhancing mass, 6.5 cm in the lower pole RK | None | RCC suspected | Nephrectomy f/b diagnosis f/b medical Mx |
| Dufour 2012 (18) | 67-year-old male with MSK, CNS and renal involvement; cANCA/anti-PR3 (+) | None | Exophytic 4 cm hypoenhancing mass LK | None | None | Medical Mx; Pt dies due to flare disease |
| Ward 2014 (19) | 48-year-old female with headache and vomiting; transient, low-level cANCA (+) (1:20) | None | RK 11 cm hypoenhancing cortical mass in upper/central region | None | Pt had parasellar mass and consolidation in lung | Rt nephrectomy f/b diagnosis f/b medical Mx |
| Vandergynst 2015 (16) | 23-year-old female with polyuria, polydipsia central DI with pituitary mass due to GPA; pANCA/anti-MPO (+) | CEUS showed 2 cm RK upper pole mass which increase to 4.3 cm on F/U | None | None | FDG PET CT initially diagnosed renal mass; F/U PET showed size increase and new LK small lesions | Diagnosis on biopsy; Rituximab for MX; F/U US 5 and 13 weeks showed resolution of lesions |
| Reeders 2017 (20) | 46-year-old male with abnormal LFT; cANCA/anti-PR3 (+) | Left renal mass incidentally detected | Lobulated mass LK with perinephric stranding | None | Chest X-ray showed numerous nodules mistaken for metastasis; biopsy renal lesion showed RCC | Nephrectomy specimen showed simultaneous presence of inflammatory lesions confused with IgG4 in perinephric area |
| Xu 2017 (21) | 55-year-old male with Gross hematuria; percussion tender over left renal region; cANCA (+), elevated PR3 | None | An ill-defined hypodense mass (maximum diameter 4.2 cm) with annular enhancement in the middle and lower pole of shrunken LK; enlarged lymph nodes at the renal hilum | None | None | Nephrectomy f/b medical Mx |
| Boncoraglio 2021 (22) | 47-year-old male with dysuria, pelvic discomfort and low-grade fever; cANCA-PR3 (+) | None | Hypoenhancing 3.8 cm× 4.0 cm mass in the lower pole of left kidney | Same | Also had IgG4 related disease in the kidney, diagnosed from the same renal biopsy | None |
| Tiwari 2021 (23) | 60-year-old female with intermittent fever, night sweats, nasal congestion, decreased appetite, and weight loss; anti-MPO (+) | Hypoechoic lesion in the right kidney | Large, wedge shaped solid, non-enhancing hypodense area at the lower-mid pole of RK, suggestive of a mass | None | None | FDG avid on PET/CT |
| Lo Gullo 2014 (24) | 38-year-old male with low grade fever, migratory arthromyalgia and dry cough; cANCA (+) |
Solid, heterogeneous left renal mass | Ill-defined, hypoenhancing renal mass | None | RCC with pulmonary metastases suspected | FDG avid on PET/CT; diagnosis on biopsy |
| Dai 2021 (25) | 32-year-old male with fever, cough, left lumbalgia; cANCA (+) | None | Tumor like left renal mass and pulmonary nodules | Tumor like left renal mass | None | FDG avid on PET/CT; diagnosis on biopsy |
| Yamamoto 2021 (26) | Male patient in his 60s with incidentally discovered left renal mass; history of Sjogren and pneumoconiosis; ANCA unknown | None | Hypovascular mass with unclear borders and para-aortic lymphadenopathy | T1 isointense, T2 hypo-to-isointense, mild diffusion restriction | USG guided biopsy nonconclusive; diagnosed on left nephrectomy | None |
ANCA, anti-neutrophil cytoplasmic antibody; B/L, bilateral; cANCA, cytoplasmic ANCA; CEUS, contrast-enhanced ultrasound; CT, computed tomography; DI, diabetes insipidus; f/b, followed by; FDG, fluorine-18 fluorodeoxyglucose; FNAC, fine needle aspiration cytology; F/U, follow-up; HU, hounsfield units; IgG4, immunoglobulin G4; LK, left kidney; MPO, myeloperoxidase; MRI, magnetic resonance imaging; Mx, management; p-ANCA, perinuclear ANCA; PCS, pelvic collecting system; PET, positron emission tomography; PR3, proteinase 3; Pt, patient; RCC, renal cell carcinoma; RK, right kidney; Rt, right; s/o, suggestive of; TCC, transitional cell carcinoma (urothelial carcinoma); USG, ultrasound; Tc99m, technetium 99m.
Table 3
| Modality | Most common findings |
|---|---|
| Ultrasound | Hypoechoic, hyperechoic or heterogenous |
| Hypoechoic mass with hyperechoic rim | |
| Scanty flow on Doppler | |
| CT scan | Hypo to isodense cortical based mass |
| Hypoenhancing, sometimes with hyperenhancement rim | |
| MRI | T1 isointense, T2 hypointense and hypoenhancing and mildly restricting on diffusion |
| PET scan | FDG avid |
CT, computed tomography; FDG, fluorine-18 fluorodeoxyglucose; MRI, magnetic resonance imaging
Discussion
GPA is a rare disease with an estimated overall incidence ranging from between 0.5–20 cases/million and prevalence ranging from 20 to 160 cases/million (1). Patients generally present with fever, weight loss, ear pain or recurrent sinusitis (2). This autoimmune systemic disorder can have a multisystem involvement, majorly lungs and kidney. Other organs like skin, orbit and GI system may also be involved (20). Renal involvement, as a mass forming pseudotumor is extremely rare, and can be a diagnostic challenge. It is difficult to differentiate it from renal cell carcinoma (3). GPA increases the odds of having RCC, further adding to the difficulty (27). In the past, these masses were confused with lymphoma, abscess, tuberculosis, IgG4 disease, Erdheim-Chester or other inflammatory pseudotumors (20,21,28). The imaging findings of the published proven GPA renal psedomasses has been described. Due to rarity of the disease, this review does not have images. However, this review aims to summarize the described cases, with emphasis summarize the described imaging findings.
On imaging, masses can be unilateral or bilateral, they can be single or multiple (11). Only two cases previously had unilateral multiple masses (3,8). Ultrasound is a good initial diagnostic modality and lesions are solid appearing. Lesions can be hypoechoic, hyperechoic or heterogenous. Verswijvel found a hypoechoic mass with hyperechoic rim (9). On Doppler, they generally have scanty flow (10). Vandergheynst et al. used CEUS to follow up these masses (16).
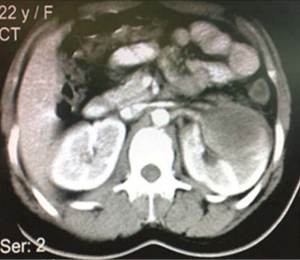
CT scan shows a hypo or isodense mass (9,10). Shape maybe round, irregular or it can take the shape of renal outline (8,10,17). Size varies from 2–11 cm with average size being 3–5 cm (13,19). Location is most commonly in the cortex and rarely can be exophytic (18). Characteristically they are hypoenhancing, compared to the rest of the renal parenchyma on contrast scans. In three cases, central hypoenhancement with rim hyperenhancement was seen (9,10,21). A representative image is provided in Figure 1.
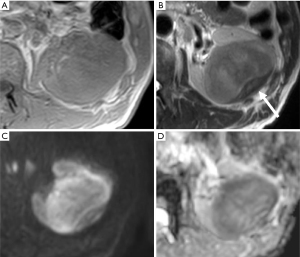
Data on MR imaging in these patients is scarce. Only three cases described using MR imaging for evaluation. Verswijvel described the lesions as T1 isointense, T2 hypointense and hypoenhancing on contrast scans. Lesions were mildly restricting on diffusion (Figure 2). Abdominal lymph nodes can be seen, which was only seen by Xu et al. (21).
PET scan shows masses as FDG avid lesions. PET can be used for diagnostic screening in known GPA patients, to detect lesions at other locations. It also helps detect response to treatment in patients with medical management (16).
There are no definite imaging clues to differentiate these pseudotumors from malignant lesions like renal cell carcinoma (RCC) or lymphoma and other inflammatory mass like lesions like abscess, IgG4 disease. However, T2 hypointensity, hypoenhancement and poor diffusion restriction, can help differentiate from RCC (clear cell variant), but differentiation from papillary and chromophobe variant can be difficult, and clinical history may give a clue. Hard to differentiate from lymphoma, but no significant restriction on diffusion can be helpful clue. Based on the enhancement pattern, an abscess was less likely. Differentiation from other pseudotumors due to IgG4 disease, Erdheim-Chester or other vasculitis could only be made possible clinically or on biopsy.
Medical management in GPA involves treatment with cyclophosphamide or rituximab, steroids, and symptomatic treatment. Four cases showed renal mass to resolve at imaging (USG or CT scan) post medical management. Post medical management, imaging at 6 months seems ideal to check for remission (2,9,13,16).
Final diagnosis required either biopsy or nephrectomy. Though imaging may not be diagnostic, but it can surely hint towards benign pathology and supplement biopsy results. In patients with renal masses and clinically having suspicion of GPA, imaging (MR and PET) complemented with biopsy should be utilized for diagnosis, so that these patients are subjected to less surgical morbidity.
Conclusions
GPA is a rare multisystemic autoimmune disorder. Renal manifestation as a pseudotumor can be a diagnostic challenge. This summary review can help guide radiologists and clinicians in known GPA patients with atypical renal masses and pathology, to always keep a GPA pseudotumor as a differential consideration.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://amj.amegroups.com/article/view/10.21037/amj-21-50/rc
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-21-50/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-21-50/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Panupattanapong S, Stwalley DL, White AJ, et al. Epidemiology and Outcomes of Granulomatosis With Polyangiitis in Pediatric and Working-Age Adult Populations In the United States: Analysis of a Large National Claims Database. Arthritis Rheumatol 2018;70:2067-76. [Crossref] [PubMed]
- Frigui M, Ben Hmida M, Kechaou M, et al. Wegener's granulomatosis presenting as multiple bilateral renal masses: case report and literature review. Rheumatol Int 2009;29:679-83. [Crossref] [PubMed]
- Roussou M, Dimopoulos SK, Dimopoulos MA, et al. Wegener's granulomatosis presenting as a renal mass. Urology 2008;71:547.e1-2. [Crossref] [PubMed]
- Maguire R, Fauci AS, Doppman JL, et al. Unusual radiographic features of Wegener's granulomatosis. AJR Am J Roentgenol 1978;130:233-8. [Crossref] [PubMed]
- Schapira HE, Kapner J, Szporn AH. Wegener granulomatosis presenting as renal mass. Urology 1986;28:307-9. [Crossref] [PubMed]
- Schydlowsky P, Rosenkilde P, Skriver E, et al. Wegener's granulomatosis presenting with a tumor-like lesion in the kidney. Scand J Rheumatol 1992;21:204-5. [Crossref] [PubMed]
- Smith DJ, Milroy CM, Chapple CR. An unusual renal mass: ?Wegener's granulomatosis. Br J Urol 1993;72:980-1. [Crossref] [PubMed]
- Fairbanks KD, Hellmann DB, Fishman EK, et al. Wegener's granulomatosis presenting as a renal mass. AJR Am J Roentgenol 2000;174:1597-8. [Crossref] [PubMed]
- Verswijvel G, Eerens I, Messiaen T, et al. Granulomatous renal pseudotumor in Wegener's granulomatosis: imaging findings in one case. Eur Radiol 2000;10:1265-7. [Crossref] [PubMed]
- Ruiz Carazo E, Medina Benitez A, López Milena G, et al. Multiple renal masses as initial manifestation of Wegener's granulomatosis. AJR Am J Roentgenol 2001;176:116-8. [Crossref] [PubMed]
- Kapoor A, Balfour-Dorsey RA, George DL. Wegener's granulomatosis presenting as multiple kidney masses. Am J Med 2002;112:82-3. [Crossref] [PubMed]
- Mohammadi Sichani M, Hadi M, Talebi A, et al. Renal Solid Mass as a Rare Presentation of Wagener's Granulomatosis: A Case Report. Case Rep Urol 2012;2012:793014. [Crossref] [PubMed]
- Leung N, Ytterberg SR, Blute ML, et al. Wegener's granulomatosis presenting as multiple bilateral renal masses. Nephrol Dial Transplant 2004;19:984-7. [Crossref] [PubMed]
- Krambeck AE, Miller DV, Blute ML. Wegener's granulomatosis presenting as renal mass: a case for nephron-sparing surgery. Urology 2005;65:798. [Crossref] [PubMed]
- Negi A, Camilleri JP, Matthews PN, et al. Wegener's granulomatosis presenting as a disappearing renal mass. Rheumatology (Oxford) 2006;45:1554. [Crossref] [PubMed]
- Vandergheynst F, Kazakou P, Couturier B, et al. From polyuria to renal mass: an unexpected link. Am J Med 2015;128:e15-8. [Crossref] [PubMed]
- Boubenider SA, Akhtar M, Nyman R. Wegener's granulomatosis limited to the kidney as a masslike lesion. Nephron 1994;68:500-4. [Crossref] [PubMed]
- Dufour JF, Le Gallou T, Cordier JF, et al. Urogenital manifestations in Wegener granulomatosis: a study of 11 cases and review of the literature. Medicine (Baltimore) 2012;91:67-74. [Crossref] [PubMed]
- Ward A, Konya C, Mark EJ, et al. Granulomatosis with polyangiitis presenting as a renal tumor. Am J Surg Pathol 2014;38:1444-8. [Crossref] [PubMed]
- Reeders J, Mani A. Granulomatosis with polyangiitis presenting as a renal mass mimicking immunoglobulin G4-related disease. Hum Pathol Case Rep 2017;10:69-73. [Crossref]
- Xu H, Zhang J, Wang Y, et al. Clinicopathological analysis of renal inflammatory pseudotumors presenting as the unilateral solitary masses. Int J Clin Exp Pathol 2017;10:7734-42. [PubMed]
- Boncoraglio MT, Prieto-González S, Fernandes-Serodio J, et al. Simultaneous presentation of granulomatosis with polyangiitis (GPA) and immunoglobulin G4-related disease (IgG4-RD). Leaving an open question: widening the spectrum of a single disease or real overlap? Mod Rheumatol Case Rep 2021;5:108-12. [Crossref] [PubMed]
- Tiwari V, Raman A, Gupta A, et al. Granulomatosis with Polyangiitis Masquerading as Renal Mass: Case Report and Literature Review. Indian J Nephrol 2021;31:406-9. [Crossref] [PubMed]
- Lo Gullo A, Bajocchi G, Cassone G, et al. Granulomatosis with polyangiitis presenting as a renal mass successfully treated with rituximab. Clin Exp Rheumatol 2014;32:S138. [PubMed]
- Dai H, Li F, Huang R. Unusual unilateral renal mass with pulmonary multiple nodules as the initial presentation of granulomatosis with polyangiitis. Hell J Nucl Med 2021;24:161-2. [PubMed]
- Yamamoto T, Tkahata K, Kamei S, et al. Granulomatosis with polyangiitis presenting as a solitary renal mass: A case report with imaging and literature review. Radiol Case Rep 2021;16:736-41. [Crossref] [PubMed]
- Tatsis E, Reinhold-Keller E, Steindorf K, et al. Wegener's granulomatosis associated with renal cell carcinoma. Arthritis Rheum 1999;42:751-6. [Crossref] [PubMed]
- Clements MB, Farhi J, Schenkman NS. Erdheim-Chester Disease Presenting as a Solid Renal Mass. Urology 2017;100:e1-e2.
Cite this article as: Khatri GD, Oztek MA. Granulomatosis with polyangiitis presenting as renal mass: a literature review of imaging findings. AME Med J 2022;7:19.

