
Polytrauma patient with lateral thoracic spondyloptosis: case report and literature review
Introduction
Cases of polytrauma are inherently difficult to evaluate and can be even more challenging to manage as extreme mechanisms of injury create an indescribable variety of pathologies. Polytraumatic injuries can range from being relatively benign and self-resolving to severe and life-threatening. Of these injuries, spinal trauma is found in up to 30% of all polytrauma cases, many with associated spinal cord injuries (SCI) causing high mortality rates (1).
Treatment of polytrauma requires a tailored focus on the injuries with the greatest potential for irreversible complications and death. Typically, injury to vital organ systems take precedence over SCI. After immediate life-sustaining treatments and patient stabilization, the concern becomes more preventative in nature and focused on minimizing long-term sequelae. These preventative measures typically involve spinal stabilization for further spinal surgery at a later date, however, this decision depends on the surgeon’s experience, preference, as well as subtleties within each patients presentation and their individual wishes (2). Pertaining to this case traumatic lateral spondyloptosis is a rare pathology as the force required is often incompatible with survival. These injuries rarely occur in isolation and almost always cause significant long-term physical disability (1-7). There is a relative paucity of case reports in the literature for traumatic spondyloptosis, especially in the thoracic vertebrae. This leaves many unanswered questions for physicians about how to most efficiently identify and treat these rare injuries.
The immediate care of acute pathologies is often the sole focus in trauma care. Long term physical and psychosocial sequelae are often neglected; however, they can be similarly important for survivors of debilitating polytrauma. In this case we address both a unique combination of polytrauma as well as the long term associated physical and psychological complications. Our goal for this case report is to highlight the need for improved treatment of significant traumatic spondylolisthesis as well as planning to support the patient as the cope with the grim prognosis. We present the following case in accordance with the CARE reporting checklist (available at https://amj.amegroups.com/article/view/10.21037/amj-22-14/rc).
Case presentation
A 24-year-old male with no significant past medical history presented to a level one trauma center as a priority 2 trauma activation as a pedestrian struck by motor vehicle travelling approximately 50 miles/h. Trauma activation was upgraded to priority 1 upon arrival and initial evaluation. Emergency medical services (EMS) reported that the patient was initially responsive on scene. Vitals obtained in the field by EMS included a Glasgow Coma Score (GCS) of 13, systolic blood pressure (SBP) in the 130 s and a heart rate (HR) in the low 100 s bpm. He was noted to have obvious facial injury and right lower extremity deformity. He was placed in a cervical collar and on a spine board for transport.
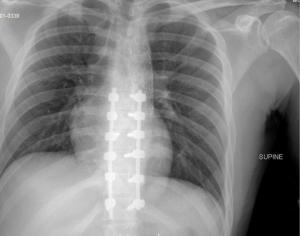
Upon arrival to the trauma center, his vitals were stable and consistent with those obtained in the field. He was able to state his name and complained of abdominal and facial pain. He also stated “I can’t feel my legs.” He was unable to provide any further meaningful information regarding the event, and was assigned a GCS of 12 at this time. Primary survey revealed a patent airway as he was speaking without respiratory distress. Physical examination revealed abrasions about face, right hip, and obvious deformity of right leg with overlying small laceration about the anteromedial tibia. He was observed to have spontaneous purposeful movement of bilateral upper extremities and flaccid bilateral lower extremities. Chest radiograph revealed a widened mediastinum and fracture dislocation of the thoracic spine at the T9-10 disc space (Figure 1). Pelvis radiograph revealed a pubic symphysis diastasis and rami fractures with suspicion for widening of sacroiliac joint.

Soon after the primary survey, the patient decompensated and became unresponsive. He was hemodynamically unstable with SBP in the 70 s with a HR in the 140 s. Rapid sequence intubation was successfully performed and mass transfusion protocol (MTP) was initiated. A pelvic binder was placed. Hemodynamics were stabilized after one round of MTP and full trauma CT scans were obtained including the head, face, entire spine, chest, abdomen and pelvis. CT identified multiple injuries including a 3-cm descending aortic arch injury with pseudoaneurysm with mediastinal hematoma, multiple bilateral rib fractures with hemopneumothorax, hemoperitoneum and retroperitoneal hematoma without obvious expansion, grade 1 segment 7 liver laceration, bilateral renal laceration versus infarct, small bowel thickening suggestive of ischemia, bilateral pubic rami fractures, bilateral sacroiliac widening with elevation of left hemipelvis concerning for vertical shear pelvic ring injury, and T9/10 lateral spondyloptosis with near complete cord transection as noted on follow up MRI.
The patient underwent thoracic endovascular aortic repair (TEVAR) with a 20 cm graft. Lactate was used as an indicator of adequate resuscitation and was noted to have normalized approximately nine hours after arrival. Spinal injury was treated with T9 laminectomy, reduction of the T9-10 dislocation, followed by T7-12 posterolateral fusion and dural repair approximately 16 hours after initial arrival. Near complete spinal cord transection was observed intraoperatively. The patient remained non-weight bearing on bilateral lower extremities given his pelvic ring injury. He had no sensation distal to the umbilicus, no motor function below the waist, no bowel or bladder control, thus consistent with American Spinal Injury Association (ASIA) A complete SCI.
Secondary survey and complete radiographs revealed left knee instability suggestive of multi-ligamentous injury, and the knee was placed in an immobilizer. An oblique mildly comminuted right ulna fracture was acutely placed into a sugar tong splint. Initial course was complicated by COVID-19 infection and acute respiratory distress syndrome which delayed surgical intervention for the pelvis injury. On hospital day 7, he underwent open reduction internal fixation (ORIF) of pubic symphysis, ORIF of the right ulna, closed reduction and percutaneous pinning of left posterior pelvic ring with trans-sacral trans-iliac screw in S2 due to sacral dysmorphism.
His post-operative hospital course involved prolonged intubation for 10 days with complications of tracheobronchitis and hospital acquired pneumonia. He required additional transfusions of packed red blood cells for acute blood loss anemia. He had dysphagia after extubation requiring tube feeds, and he eventually progressed to a regular diet. His mental status slowly improved over the course of his stay, but he had a persistent flat affect. He was eventually transferred to subacute rehabilitation 23 days after initial presentation.
After discharged from the hospital, he had intermittent follow-up with orthopedics as he often missed appointments. At 3-month post-injury follow-up his use of the left knee brace was found to be inconsistent and incorrectly applied. Radiographs at that time demonstrated significant posterior lateral subluxation of the left knee as a result of his multi-ligamentous knee injury with inadequate bracing. He had intact distal pulses at time of the encounter. The remainder of his fractures were healing appropriately without any concern. He was admitted to the hospital directly for reduction and fixation of the left knee. The following day, he underwent open reduction of the right knee with multiplanar external fixation. The external fixator was in place and in good position as confirmed on intraoperative fluoroscopy. The external fixator was to remain in place for 2–3 months to allow for stability of the knee. He eventually returned for follow-up at 6 months post-operatively and subsequently underwent removal of external fixator. Examination under anesthesia after removal revealed 10–80° knee flexion which was similar to the contralateral.
In the interim, the patient has struggled with behavioral issues reported by the rehabilitation facility. He frequently declined care including physical therapy, occupational therapy, repositioning, hygiene, wound care, and specialists’ follow-up appointments. The patient declined prescribed medications and treatment, specifically antidepressants and psychiatric care/counseling. Multiple instances of violent verbal outbursts with staff and one instance of physical violence were reported. Complications that have occurred in the 26 months since initial injury include decubiti of the sacrum, left greater trochanter and the left heel. He developed flexion contractures of bilateral hips with increasing heterotopic ossification (HO) and equinus contracture of the left ankle. Imaging at 2 year follow up shows persistent stability and alignment of the thoracic spine (Figure 2). Additionally, severe HO of bilateral hip is evident on imaging in advanced stages resulting in ankylosis of the hips.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Literature review
In an attempt to identify all cases of lateral thoracolumbar spondyloptosis, a comprehensive literature search was performed. PubMed, Embase, and Scopus (last accessed 4/30/22) were utilized to search for the following terms: “lateral thoracolumbar spondyloptosis” OR “lateral thoracolumbar grade 5 spondylolisthesis”. The search included all articles published before 5/1/22. The inclusion criteria were articles that reported patients who suffered from acute lateral thoracolumbar spondyloptosis with neurologic status immediately following the injury, detailed surgical treatment, and neurologic status following treatment. Exclusion criteria were cadaveric studies, review articles, technique articles, and articles that did not report neurologic outcomes. One author performed the initial search, and a second author independently screened the search results to identify articles that met the inclusion criteria. The references of the included studies were further reviewed to identify any other relevant papers that may have been missed by the initial search.
Discussion
Polytrauma cases, especially when complicated by SCI, continue to be particularly challenging despite numerous diagnostic and therapeutic advancements. Having a structured approach is necessary to rule out or treat the most life-threatening pathologies first prior to assessing for non-life-threatening disabilities.
Spinal instability and SCI are not the first pathologies assed but quickly rise to the top of the list of clinical concerns due to the bleak outcomes with significant neurologic deficit. The threshold for ordering diagnostic testing to asses spinal pathologies is very low to minimize cases going undetected and progressing to severe neurological damage or death (3). Plain radiographs of the chest and pelvis are generally obtained on arrival for high priority trauma patients and may be useful as a quick and relatively sensitive assessment of significant acute bony spinal abnormalities. If there remains a high clinical suspicion following a negative radiograph, further imaging such as CT or MRIs may be indicated (8). Polytrauma patients with spinal instability in the setting of multiple organ system involvement is an indication for immediate surgical intervention during initial resuscitation. Delayed spinal stabilization in polytrauma cases with SCI have been correlated with increased risk of death and long-term complications (1,9). Early intervention for spinal stabilization has been shown to reduce overall length of hospital and intensive care unit stays, lower this risk of sepsis, decrease the number of days requiring mechanical ventilation, and decreased the risk for other long-term complications (8).
Spondyloptosis, or grade 5 spondylolisthesis, is the most severe form of spondylolisthesis, as two adjacent vertebrae are shifted 100% out of position with regards to one another in the vertical plane. Most instances of spondylolisthesis occur due to gradual degeneration; however, the most severe cases are more likely to be seen in high energy traumatic accidents (8). Most cases of spondyloptosis occur in the sagittal plane while lateral spondyloptosis, in the coronal plane, is extremely rare (3,6,10). Spondyloptosis causes dramatic spinal instability with a high likelihood of devastating neurological compromise. According to our review there have been 13 cases of traumatic lateral thoracolumbar spondyloptosis reported in the literature (2,4,11-13). Of all reported cases, complete neurologic deficits have been observed in all but two (2-10,14). An outline of these cases, the patients’ neurologic status and their treatments can be found in Table 1. These injuries are typically associated with other musculoskeletal pathologies including rib fractures and flail chest due to the anatomy and the high-energy mechanism of injury that is required (12,15). Current recommendations for spondyloptosis include operative management with fusion and possible decompression as early as possible to restore spinal stability and preserve any remaining neurologic function. Surgery can be delayed secondary to other injuries that complicate the logistics of orthopaedic surgical intervention. This raises concerns regarding the association between delays in management and worse outcomes. The paucity of data regarding such a rare pathology has yet to provide a consensus on the optimal surgical technique. Anterior, posterior, or combined approaches have been employed previously, but success rates of restoring neurologic function has been bleak with any option (4-15). In our case posterior fusion was preformed within 24 hours of the injury, however, neurologic function below the umbilicus was not recovered.
Table 1
| Article | Number of patients | Neurologic status | Treatment |
|---|---|---|---|
| Cabrera et al. | 1 | ASIA B on presentation, improved to ASIA D at one-year post injury | Combined anterior and posterior approach with corpectomy expandable cage of L2–L4 |
| Yadla et al. | 5 | All 5 patients were ASIA A on presentation, 4 out of 5 remained ASIA A with one patient recovering to ASIA C | 2 patients underwent isolated posterior fusion. 3 patients were treated with combined posterior and anterior decompression and fusion |
| Garg et al. | 5 | All 5 patients were ASIA A on presentation, all 5 remained ASIA A after treatment | All 5 were treated with an isolated posterior approach with decompression and fusion |
| Bellew & Bartholomew | 1 | ASIA D on presentation with cauda equina, improved to ASIA E after treatment | Posterior decompression and fusion of T12-L5 |
| Jindong & Qing | 1 | ASIA A at time of injury, improved to ASIA C at one-year post injury | Combined anterior and posterior approach with decompression and fusion of T12-L4 |
ASIA, American Spinal Injury Association.
A chronic complication that this patient has incurred that is often associated with SCI was HO. This is when soft tissues such as muscle, tendons, and ligaments incur bony like infiltration. HO is a known potential complication following a traumatic brain or SCI with an incidence of 11–20% (16). HO can result in significant discomfort, impingement with resulting pain, sensory abnormalities, joint contractures, and motor dysfunction. The mechanism for development of neurologic HO is poorly understood, but is thought to be the result of central nervous system injury redirecting ectopic bone formation inside soft tissue structures. Treatment options may include prophylaxis with agents such as bisphosphonates, or less favorable off label use of non-steroidal anti-inflammatory drugs, and targeted radiation. Physiotherapy may be used as an adjunct although it has not been shown to be preventative. Ultimately surgical intervention may be required to improve mobility and hygiene once the HO has matured, typically 1-year post SCI. The overall prognosis is poor, specifically in cases with high grade HO and limited neurologic function (16).
Lastly as depicted in this case, providers need to be aware of the association of psychiatric illness in the polytrauma patient. Depression, anxiety, post-traumatic stress disorder (PTSD), suicidality, and overall mental health decline are all found to be associated with patients experiencing traumatic injuries. Previous research has found that there is a significant correlation between the severity of traumatic disability and the development of either depression or PTSD (17). In a study conducted by Vranceanu et al., it was found that 23% of patients developed clinical depression in the short-term following significant trauma while 28% developed PTSD. Further, more than a quarter of the variance in pain and disability found in patients with similar trauma can be explained by psychological variables (18). These risks increase in patients who suffered head trauma, are physically impaired from the trauma, or who must cope with dramatic lifestyle or other changes secondary to their trauma. Data has also shown that patients with a traumatic injury history who subsequently develop psychiatric illnesses are at higher risk for repeated hospital admissions due to these associated psychiatric complaints. Of these illnesses, substance use disorders and psychotic disorders are the most common reasons for psychiatric-related hospital admissions. Additionally, these patients are at significantly higher risk for suicide with up to 30% of these patients having at least one suicide attempt in their lifetime. This is in comparison to the United States national average lifetime risk for a suicide attempt being reported between 2–5% (18,19). These psychiatric issues highlight the lifelong struggle that many patients face as a result of their physical trauma. Implementing mental health support for these patients as early as possible after acute stabilization can be crucial. Previous data has indicated that a “mind-body-skills” based intervention can be feasibly adopted into trauma care systems and early indications show that it can be efficacious in reducing overall pain and disability for these patients (19).
Polytrauma cases are inherently unique and should be managed on a case-by-case basis with a multidisciplinary approach based on the organ systems affected. The discussion on how to sort particular injuries based on priority is beyond the scope of this paper, but we emphasize the importance of addressing spinal instability as early as possible. Given the rarity of lateral spondyloptosis as discussed in this case, there is a need for more data to optimize its management. Using guideline for management of more common traumatic spinal injuries is appropriate at this time in order to attempt to preserve any neurologic function. We also hope to emphasize the importance of addressing possible long term physical and mental complications that are present in a large percentage of the trauma cohort.
We recognize that this case report depicts a patient who experienced a unique combination of injuries. Lateral spondyloptosis is very rare condition with few examples in the literature. Additionally, the patient presented here had a similarly poor outcome in comparison to other cases in the literature. This makes it challenging to surmise any recommendations for treatment directly. Other limitation specific to our particular case include the patient’s inconsistent follow up. There are gaps in his follow up as he missed numerous medical treatments. This variable presents the question of if his course would have been different if he followed all medical advice.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://amj.amegroups.com/article/view/10.21037/amj-22-14/rc
Peer Review File: Available at https://amj.amegroups.com/article/view/10.21037/amj-22-14/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://amj.amegroups.com/article/view/10.21037/amj-22-14/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mugesh Kanna R, Prasad Shetty A, Rajasekaran S. Timing of intervention for spinal injury in patients with polytrauma. J Clin Orthop Trauma 2021;12:96-100. [Crossref] [PubMed]
- Cabrera JP, Yankovic W, Luna F, et al. Traumatic spondyloptosis of L3 with incomplete neurological involvement: A case report. Trauma Case Rep 2019;24:100248. [Crossref] [PubMed]
- Aspinall P, Harrison L, Scheuren P, et al. A Systematic Review of Safety Reporting in Acute Spinal Cord Injury Clinical Trials: Challenges and Recommendations. J Neurotrauma 2021;38:2047-54. [Crossref] [PubMed]
- Yadla S, Lebude B, Tender GC, et al. Traumatic spondyloptosis of the thoracolumbar spine. J Neurosurg Spine 2008;9:145-51. [Crossref] [PubMed]
- Cherian I, Dhawan V. Lateral lumbar spondyloptosis. Int J Emerg Med 2009;2:55-6. [Crossref] [PubMed]
- Barwar N. Post-traumatic L4-L5 spondyloptosis with cauda equina syndrome: A case report. Trauma Case Rep 2021;33:100475. [Crossref] [PubMed]
- Gertzbein SD, Offierski C. Complete fracture-dislocation of the thoracic spine without spinal cord injury. A case report. J Bone Joint Surg Am 1979;61:449-51. [Crossref] [PubMed]
- Sjeklocha L, Gatz JD. Traumatic Injuries to the Spinal Cord and Peripheral Nervous System. Emerg Med Clin North Am 2021;39:1-28. [Crossref] [PubMed]
- Wong KR, Mychasiuk R, O'Brien TJ, et al. Neurological heterotopic ossification: novel mechanisms, prognostic biomarkers and prophylactic therapies. Bone Res 2020;8:42. [Crossref] [PubMed]
- Bliemel C, Lefering R, Buecking B, et al. Early or delayed stabilization in severely injured patients with spinal fractures? Current surgical objectivity according to the Trauma Registry of DGU: treatment of spine injuries in polytrauma patients. J Trauma Acute Care Surg 2014;76:366-73. [Crossref] [PubMed]
- Garg M, Kumar A, Sawarkar DP, et al. Traumatic Lateral Spondyloptosis: Case Series. World Neurosurg 2018;113:e166-71. [Crossref] [PubMed]
- Bellew MP, Bartholomew BJ. Dramatic neurological recovery with delayed correction of traumatic lumbar spondyloptosis. Case report and review of the literature. J Neurosurg Spine 2007;6:606-10. [Crossref] [PubMed]
- Ver MLP, Dimar JR 2nd, Carreon LY. Traumatic Lumbar Spondylolisthesis: A Systematic Review and Case Series. Global Spine J 2019;9:767-82. [Crossref] [PubMed]
- Chandrashekhara SH, Kumar A, Gamanagatti S, et al. Unusual traumatic spondyloptosis causing complete transection of spinal cord. Int Orthop 2011;35:1671-5. [Crossref] [PubMed]
- Jindong Z, Qing L. Traumatic lateral spondyloptosis of L2 with complete neurological deficit: A case report. Trauma Case Rep 2020;29:100339. [Crossref] [PubMed]
- Cipriano CA, Pill SG, Keenan MA. Heterotopic ossification following traumatic brain injury and spinal cord injury. J Am Acad Orthop Surg 2009;17:689-97. [Crossref] [PubMed]
- Nota SP, Bot AG, Ring D, et al. Disability and depression after orthopaedic trauma. Injury 2015;46:207-12. [Crossref] [PubMed]
- Vranceanu AM, Bachoura A, Weening A, et al. Psychological factors predict disability and pain intensity after skeletal trauma. J Bone Joint Surg Am 2014;96:e20. [Crossref] [PubMed]
- Joe S, Baser RE, Breeden G, et al. Prevalence of and risk factors for lifetime suicide attempts among blacks in the United States. JAMA 2006;296:2112-23. [Crossref] [PubMed]
Cite this article as: Lucasti C, Morgan D, Slowinski J, Maraschiello M, Kowalski J. Polytrauma patient with lateral thoracic spondyloptosis: case report and literature review. AME Med J 2022;7:30.

